Nissen, Rudolph (1896–1981), Swiss (German-born) surgeon. From 1920 to 1933 Nissen held a series of surgical positions at the universities of Breslau, Freiburg, Munich, and Berlin. From 1933 to 1939 he served as professor of surgery and head of the department at the University of Istanbul. After extended stays at hospitals in New York City, he emigrated to Basel, Switzerland, to become a professor of surgery at the university and chief surgeon at Burgerspital. He authored or coauthored over 30 books on surgery and 475 papers on thoracic and abdominal surgery. He first performed the fundoplication associated with his name in 1951 on a patient with a hole in the esophageal sphincter; in 1956 he proposed the surgical procedure for the treatment of reflux of gastric contents due to improper functioning of the lower esophageal sphincter. Nissen is also credited with performing the first total pneumonectomy in 1931.
.
Ten Questions, Parents Needs to Ask Before Fundoplication Surgery
by Susan Agrawal
The following questions are intended to help parents and doctors determine how risky a fundoplication surgery would be for a specific child. Each question discusses a condition or state that may make a fundoplication more likely to have complications.
1. Does my child have a motility problem?
Many children with reflux also have concurrent motility problems, such as delayed gastric emptying, dysmotility, or an oesophagal motility problem. If your child has a diagnosed motility problem, fundoplication surgery will not change the motility problem and usually, in fact, makes it worse. A study by top motility specialists demonstrated that almost all children with functional GI symptoms had abnormal motility after anthro duodenal manometry testing and that the group of children who had had a fundoplication surgery to relieve their symptoms continued to have the same symptoms after surgery. 1 In many cases, symptoms of a motility problem are mistaken for reflux when in fact the motility problem is the underlying cause of most symptoms. Since fundoplications make the stomach smaller, children with delayed emptying may have even slower emptying.
While some surgeons perform a simultaneous pyloroplasty to deal with this problem, this second surgery has its own risks and complications. Similarly, children with oesophagal motility problems who have trouble swallowing may have even more problems after surgery since fundoplication tightens the junction between the oesophagus and stomach, worsening mobility in many children. All children with significant mobility problems should avoid a fundoplication if at all possible since complications such as retching, swallowing problems, and emptying appear to be much greater in this patient population. Motility medications and a GJ tube are far better options.
.
2. Have all medical treatments been tried?
Almost all studies suggest trying conservative medical treatments for reflux, including medications that reduce acid, lifestyle changes such as raising the head of the bed or thickened feeds, or medications that improve stomach emptying. Despite this recommendation, as many as 14% of patients have surgery without even seeing a GI specialist and in one study 77% of patients had not exhausted all medical treatments before surgery. 2 Failed medical management of reflux, including the failure of all PPIs to reduce acid, failure of motility medication, failure of G-tube feeds alone, and failure of lifestyle changes is a necessary prerequisite for fundoplication. Surgery should not be considered until all conservative medical treatments have been tried.
Has my child had the appropriate testing to rule out other conditions that mimic reflux? Shockingly, 14-26% of patients receiving a fundoplication have never had any basic testing to confirm reflux and rule out other disorders.
Testing should be performed to rule out gastroparesis, cyclic vomiting, rumination, and eosinophilic esophagitis, all of which mimic reflux but will not be helped by a fundoplication.
In addition, appropriate testing for reflux, particularly a pH probe or preferably an Impedance probe, should be performed to confirm reflux. The following tests are recommended at a minimum:
Upper GI to rule out anatomical problems Upper Endoscopy with biopsies to rule out Eosinophilic Esophagitis
Gastric Emptying Scan or preferably Antroduodenal Manometry to rule out a motility problem
pH probe or Impedance probe to confirm the severity of reflux
Does my child have a history of vomiting, gagging, or retching?
Cont with rest click on the link below.
http://www.articles.complexchild.com/00009.pdf
.
The goal of a fundoplication is to prevent stomach contents from returning to the oesophagus. This operation is an accomplished by wrapping the upper portion of the stomach around the lower portion of the oesophagus, tightening the outlet of the oesophagus as it empties into the stomach. After a fundoplication, food and fluids can pass into the stomach but are prevented from returning to the oesophagus and causing symptoms of oesophagal reflux. A large skin incision may not be required. In most cases, a fundoplication can be performed by a pediatric surgeon using a small telescope and miniaturised instruments placed through three to four band-aid sized incisions on the abdomen.
Why is fundoplication necessary?
Fundoplication is recommended for children who have complications or persistent symptoms related to gastroesophageal reflux (GER) that are not improved by medication. Symptoms of gastroesophageal reflux include vomiting, esophagitis (heartburn) gastroesophageal stricture, recurrent pneumonia, breathing problems, and inadequate growth. Before an operation is performed your child may have one or more tests confirming GER, such as a pH probe study or esophagogram.
How is a fundoplication performed?
This animation reveals more about why and how
Fundoplication is performed in two to three hours with a two to three-day hospital stay following surgery. Postoperative, during your child’s hospitalisation, he/she will receive intravenous fluids and pain medication. As soon as your child feels well enough he/ she will be allowed to eat, drink and take pain medication by mouth (usually 1-2 days after surgery).
In some patients, a gastrostomy tube is placed into the stomach to allow feedings to be administered and air to be released. Air release is called “venting”. It may be hard for your child to burp for many weeks after a fundoplication. Venting allows air to leave the stomach, which decreases bloating and keeps your child comfortable. During your child’s hospital stay, the bedside nurse will teach you how to vent, care for and use the gastrostomy tube.
In most fundoplication operations, there is very little blood loss. Your child will receive blood only in the rare case of an extreme emergency. If you wish to provide a directed donation of blood, contact our office, 1-2 weeks in advance of the operation.
How long will my child remain in the hospital after the operation?
Most children are ready to go home in two to three days after the operation.
Homecare
Most children are ready to go home in two to three days after the operation. Your child’s diet may be restricted for some time and they may be required to use a gastronomy tube.
Eating By Mouth
If your child is to resume his or her usual diet, it is best to start slowly. Begin with liquids, advance to soft foods, and then to a regular diet. It may take several weeks for the postoperative swelling to subside and for solid foods to pass easily into the stomach. Foods that cannot pass into the stomach will be vomited up. It is not unusual for this to occur from time to time in the first few weeks after surgery.
Gastrostomy Tube and Supplies
If your child leaves the hospital with a gastrostomy tube, a replacement tube of the same size will be sent home with you at discharge. If your child will be receiving feedings by gastrostomy, supplies will be ordered by the surgical nurse practitioner from a home care company. The home care company will ship supplies directly to your home. A nurse may come to your home, for a few visits, to help you learn to deliver feedings and take care of the gastrostomy tube. Long-term management of feedings and ordering of supplies will generally be the responsibility of your child’s gastroenterologist.
Pain Management
Prescription pain medication is not routinely required after hospital discharge. Most children only need Acetaminophen (Tylenol®) or Ibuprofen (Motrin®) once they are at home. Follow the dosage directions on the label. If your child is still uncomfortable, call our office and we may prescribe something stronger.
Care for Dressings
Gauze and clear plastic dressings, placed over the incisions, may be removed two days after surgery. Over the incision, there will be pieces of tape called Steri-strips®. On the Steri-strips®, there may be a small amount of blood. This is normal. Your child can bathe with the Steri-strips® in place. These can be removed one week after the operation. The skin surrounding the incision may be red and bruised, and the incision may be slightly swollen. This can last several weeks. There will be no visible stitches to remove because they are under the skin. The stitches will dissolve after several weeks.
In most operations, the wound is closed with dissolvable suture (stitches). These stitches are under the skin and do not have to be removed. In some children, these stitches may come through the incision about 4 weeks postoperatively. This may be associated with a little local redness and pus and it may involve an end of the incision or a larger portion. This is normal and is best treated by gently cleansing the area with soap and water and waiting. When the suture falls out or completely dissolves, the wound will heal. If your child has worsening redness, swelling pain of the incision and a fever within 2weeks of the operation, please call our office.
Healing Ridge
After the incisions are healed you will be able to feel a firm ridge just underneath. This is called a healing ridge and it is normal to find this after surgery. The healing ridge usually lasts for several months before it softens and disappears.
Bathing Restrictions
Your child may bathe or shower as soon as two days after surgery. Once your child is feeling better, before discharge or at home, he or she may bathe or shower without restriction.
Activity Restrictions
There are no specific activity restrictions following surgery. Your child can return to school as soon as he or she feels well enough.
Do I see the surgeon again after the operation?
A visit with your child’s Primary Provider and Gastroenterologist at one to two weeks after the discharge is recommended. Fundoplication may have long-term complications including gas bloat, difficulty swallowing, and unwrapping or slipping.
Diet After
fundoplication will take time for your child to recover from this operation and for food to pass comfortably into his or her stomach. To make the first 3 months more comfortable, we have developed diet suggestions to help your child.
The First 2 Weeks
After the operation, it is best to offer liquids only. Your child may not be able to burp or vomit after the operation, therefore, avoid carbonated beverages or gum. These increase air in the stomach, which can be very painful.
Suggested Diet:
Liquids include water, juice, milk, milkshakes, ice cream, jello, jelly, pudding, and pureed soups; pureed baby food and yogurt anything runny
The 3rd And 4th Weeks
After surgery, it is much easier for your child to eat more textured foods but we recommend going slowly. You can begin by offering soft foods.
Suggested Diet:
Soft foods include mashed potatoes, pasta, rice and bread, fish, crackers, cereal, ground beef, cheese, and peanut butter.
The Next 2 Months
If eating goes well, your child can slowly resume his or her usual diet with some exceptions listed below.
Suggested Diet:
Your child may eat most foods but should avoid hot dogs, steak, chicken, pizza, and nuts. These are foods that can get stuck in your child’s esophagus and may not pass into the stomach. If this happens, your child may vomit the piece of food to clear the esophagus or he or she may need to be hospitalized to remove the food. This is uncomfortable and sometimes frightening. It is best to prevent this situation, by avoiding potentially problematic foods, for the first 3 months after the operation.
Diet After Nissen Fundoplication Surgery
Very Interesting reading
This diet information is for patients who have recently had Nissen fundoplication surgery to correct reflux disease or to repair various types of hernias, such as a hiatal hernia and intrathoracic stomach. This diet may also be used for other gastrointestinal surgeries, such as Heller myotomy and repair of achalasia. The diet will help control diarrhea, excess gas and swallowing problems, which may occur after this type of surgery.
Nissen fundoplication in children, and postoperative acid reducing
Outcome after Computer-Assisted (Robotic) Nissen Fundoplication in Children Measured as Pre- and Postoperative Acid Reducing and Asthma Medications Use.
Last date: 25. May. 2016
Published: 2015-01-01
Gastroesophageal reflux is common in infants and children and most of them will outgrow their symptoms by 12 to 18 months of age. Gastroesophageal reflux disease (GERD) is pathological and can, if left untreated, result in complications such as reflux esophagitis, Barret esophagus, and esophageal stricture. GERD may also be associated with pulmonary complications, apnea, and failure to thrive. Medical treatment such as antacids and prokinetic medication is the first – line therapy and is successful in most patients. When this is insufficient, antireflux operations are considered. Previous studies have shown excellent results and low morbidity with fundoplication indicating that the operation should be performed early for children with GERD.
Laparoscopic fundoplication (LF) has now become the gold standard for surgical treatment of GERD in children and excellent symptomatic results have been shown. More and more pediatric centers around the world are now using robotic-assisted laparoscopy to perform a fundoplication. Since there is nothing robotic, i.e. automatic, about the system, we consider the term computer-assisted laparoscopic surgery (CALS) more appropriate. Although the computer-assisted technique is similar to that of conventional laparoscopy there are considerable differences, e.g. the use of 3D vision in CALS but, on the other hand, the lack of tactile response. Various studies have reported excellent short-term results and demonstrated the safety and feasibility of computer-assisted fundoplication (CAF) but so far long-term studies are scarce.
Discussion
This study demonstrates that the CAF significantly reduced the acid reflux from the stomach to the esophagus and the use of anti-reflux medication.
Laparoscopic Watson Fundoplication Is Effective and Durable in Children with Gastroesophageal Reflux
https://www.hindawi.com/journals/mis/2014/409727/
VIDEO Narrated by a World ranked Surgeon
Laparoscopic Nissen Fundoplication – Narrated – 3mm JustRight Sealer
Dr. Steve Rothenberg uses the JustRight Surgical 3mm Vessel Sealing System during a laparoscopic Nissen Fundoplication
Imaging Findings of Successful and Failed Fundoplication 2014
Postoperative imaging findings contribute to the diagnosis of successful and failed fundoplication procedures. Gastroesophageal
reflux disease, a common illness in the United States, is primarily treated medically but may require surgery if there are persistent
symptoms or reflux complications despite medical treatment. Laparoscopic. Nissen fundoplication has become the most used and successful surgical antireflux procedure since its introduction in 1991.
Radiologists should understand the anatomy of the esophagogastric junction, antireflux and esophageal protective mechanisms, and preoperative radiologic findings that contribute to the selection of the surgical technique, as well as the most commonly used antireflux operations and their indications. Barium examination and computed tomography of the thorax and abdomen play an important role in the follow-up of patients with gastric fundoplication, including evaluation of surgical effectiveness and detection and characterization of postoperative complications. Failed fundoplications are classified into six types: tight Nissen, incompetent repair, disruption of the wrap, stomach slippage above the diaphragm, slipped Nissen, and transdiaphragmatic wrap herniation. Classification is based on radiologic visualization of the obstructed esophageal lumen, recurrence of gastroesophageal reflux, integrity, and location of the gastric wrap, stomach slippage, and recurrence of a hiatal hernia. Imaging findings are useful in detecting complications, providing anatomic information to identify the cause of surgical failure, and selecting appropriate medical or surgical management.
Gastronomy and Tubes
FOR USA
Equipment/Supply Exchange Program + Resources
To connect families in need of eternal formula, pumps, tubing and other supplies with families who have items to donate.
Individuals Seeking Products to Individuals Donating Products. Products available are based solely on donations.
The Program
The Equipment/Supply Exchange Program connects
Supplies vary daily based upon what’s been donated and what’s been shipped, so check back often!
The person requesting supplies must pay for shipping prior to any products being shipped from the donor, but this should be the only cost associated with the products.
Supplies are not distributed from a central warehouse, they are shipped from Individual to Individual.
Products Typically Exchanged
Our focus is on supplies and equipment related to home tube feeding and IV nutrition. Typical items include:
Enteral formula
Feeding bags
Tubing
IV poles
Syringes
Pumps
Related supplies
We do not list prescription drugs
Procedure for Donating Supplies or Equipment
Gastrostomy tubes are feeding tubes placed through the abdomen into the stomach. Gastrostomy tubes are used to give children formula, liquids, and medicines. These tubes are placed by aPediatric Surgeon or by a Pediatric Gastroenterologist. A gastrostomy tube is placed one of two ways: 1) percutaneously and 2) surgically.
At hospital discharge, a referral will be made to have a nurse visit your home. The nurse will help you care for the gastrostomy tube and give feedings and medications and, in general, serve as a resource in your home.
Published on Jan 23, 2015
This animation reveals the placement of a percutaneous endoscopic gastrostomy – PEG, or “feeding tube” in patients who are unable to take food by mouth for an extended period of time. It demonstrates the two main surgical techniques for PEG tube placement, the “pull” method, and the “push” method.
Surgically Inserted Gastrostomy Tubes
The paediatric surgeon places a gastrostomy tube in the operating room under general anaesthesia. This operation is done through a small incision (cut) on the abdomen. The surgeon may place a temporary tube, called a Malecot®, into the gastrostomy opening. The Malecot® will be stitched to the skin and left in place for several weeks. The Malecot® allows the gastrostomy tract to heal well before a ballon type gastrostomy tube is inserted. A Malecot® tube is about twelve inches long, and most of the tube extends out of the abdomen.
After the gastrostomy tube is placed your child will remain in the hospital for observation and care. An IV (intravenous line) will be placed in the operating room before the procedure and this will be used to give fluids, antibiotics and pain medications while your child is recovering. Feedings are usually started the day after the gastronomy is placed.
(A gastrostomy is a surgical opening made in a child’s stomach to insert a feeding tube. A child may be given a gastrostomy because serious medical problems prevent him or her from eating and drinking in the usual way or from getting enough nutrients. The tube used for feeding is sometimes called a G-tube. This video discusses a variety of issues related to using a G-tube)
Changing the Malecot® To a Balloon Gastrostomy Tube
After a few weeks, the Malecot® will be removed by the surgeon or the surgical nurse and a skin level balloon gastrostomy tube will be placed. These tubes are made of silicone. They are held in the stomach by a water-filled balloon. When the nurse inserts the device, she will teach you how to take care of the tube. For more information watch the following guides:
Percutaneous Endoscopic Gastrostomy (PEG) Tube.
A PEG Tube, or Percutaneous Endoscopic Gastrostomy tube, is placed by a Pediatric Gastroenterologist in the operating room. The PEG tube is inserted using a telescopic instrument, called an endoscope. The endoscope is a small tube with a light and camera on the end that lets the Gastroenterologist see into the oesophagus (food tube) and stomach. The endoscope allows the doctor to choose the best location in the stomach to place the PEG tube. Once the location is chosen, a small opening is made on the outside of abdomen into the stomach. After the opening is made, the top part of the PEG tube is pulled up out of the stomach through this opening. The top of the tube rests on the skin and the bottom part of the PEG, which is shaped like a bulb, remains inside the stomach. This bulb shape anchors the tube in the stomach and prevents it from coming out.
After the PEG tube is placed your child will be admitted to the hospital for observation and care. The hospital stay is usually three days. Prior to the procedure, an IV (intravenous line) will be placed in the operating room. This will be used to give fluids, antibiotics and pain medication, for one to two days, as your child is recovering. Feedings will be started through the PEG tube within one or two days.
The PEG tube which is made of silicone must stay in the stomach for about three months to allow the tract (hole) to heal between the abdomen and the stomach. The tract must be well healed so it is safe for the gastrostomy tube to be changed.
I Have added this Video to just give you the Parent an idea and a few things on feeding via a tube. My own daughter is tube feed, I found this video very helpful
Taking Care of Your Child’s Gastrostomy Tube (G-Tube). Tara Spruill, RN, BSN – Nemours Children’s Clinic, Jacksonville discusses gastrostomy tube or g-tube education.
Homecare
If your child requires continuous feeding with the gastrostomy tube, a pump and supplies will be ordered by the GI or surgical nurse from a home care supply company. The equipment and supplies will be delivered to your home or to the hospital before your child is discharged. You will be taught to use the pump by a representative from the home care company or home nursing agency, as pumps differ from hospital to home. Feeding bags, replacement gastrostomy tubes, extension sets, syringes, gauze, tape and formula will be ordered for your child by the GI or surgical nurse.
General Feedings Guidelines
Give feedings and medications as directed by your nurse or doctor. Flush the gastrostomy tube with 10-15cc’s of warm water after every feeding or medication. This prevents clogging and keeps the tube as clean as possible. If you are giving continuous drip feeding into a PEG tube you may want to tape connections to prevent disconnection of the extension set from the tube and spillage of feedings. If you are using a balloon gastrostomy, such as an AMT mini-one tube, check the volume of water in the balloon every week and refill as necessary to maintain the amount of water prescribed by your child’s doctor or nurse (Do not perform this until at least 2 months after the tube was initially placed).
This video will educate families on how to properly care for a pediatric gastrostomy tube. This is just to give you the Parents an idea on how or what you need to do.
What if the tube comes out before the gastrostomy tract has healed?
It rarely happens with a PEG tube and sometimes happens with the Malecot® or balloon gastrostomy tubes. If the tube becomes accidentally dislodged call your child’s doctor
If you do not speak to a doctor or nurse after thirty (30) minutes take your child and gastrostomy supplies to the nearest emergency room for tube reinsertion. A tube will be placed into the gastrostomy tract to prevent closure and the need for another operation. If the emergency room doctors and nurses have questions, they can call the paediatric gastroenterologist, or surgeon who placed the tube.
If you do not have a replacement gastrostomy tube to take with you, a FOLEY® catheter of the same size or smaller can be inserted as a replacement tube. Often, a special x-ray called a “gastrostomy tube dye study” will need to be taken to make sure the newly placed tube is in the stomach. A FOLEY® catheter can be used for feeding and stomach decompression at home. Call your GI or surgical doctor or nurse if your child required a visit to the emergency room for care of his or her gastrostomy tube.
What should I do about the following problems?
Redness around the site
The skin may be slightly pink after initial insertion. You should see a decrease in this pink colour over time. If the skin becomes tender, warm or red, call your child’s doctor or nurse.
Crusting
Drainage that dries on the skin is called crusting. Crusting and drainage are common around gastrostomy tubes. You can remove crusting and drainage with warm water.
Bleeding
If tube gets bumped or is rubbed, there may be a small amount of bleeding from around the tube. Apply pressure should stop the bleeding for up to ten minutes. If the bleeding does not stop, call your child’s doctor or nurse. Blood coming through the tube is not normal. If this happens to call your child’s doctor or go to the nearest emergency room.
Granulation Tissue
Granulation tissue appears in most children at some time after the gastrostomy tube is placed. This tissue is common and not dangerous. It grows directly around the gastrostomy hole and looks raised, red and may ooze fluid or bleed easily. Granulation tissue should be treated when it first appears. This can be done in the office by your child’s nurse or doctor. A special ointment or cream will be prescribed to apply to the granulation tissue (not the surrounding skin) up to four times a day until the granulation tissue goes away.
Fever
If your child has a fever, call your child’s paediatrician.
Vomiting and/or diarrhea
If your child has vomiting and/or diarrhea, call your child’s pediatrician and the pediatric GI or surgical nurse or doctor for advice.
Homecare for Surgically Inserted Tubes
Skin Care With a Surgically Inserted Tube
Cleanse the area around the GT with water daily. After cleaning the skin around the gastrostomy tube dry well. If there is a Malecot® in place, make sure it is taped securely in place, to prevent movement.
AMT Mini One Gastrostomy Feeding Extension Sets
When your child has an AMT mini-one skin level button in place you will be using feeding extension sets. A feeding extension set is a special tube that connects to the gastrostomy tube and allows formula, liquids and medicines to be given into the stomach. There are two types of sets available for use with an AMT mini-one skin level tube. These are a 1) bolus set and a 2) right angle set. The bolus set is used for feedings given by gravity through a syringe. The right-angle set is used for slow or continuous feedings, given by a pump. Either tube can serve as a decompression tube to drain air or liquid from the stomach. The decompression tube is used if a child has too much gas (which can’t be burped up) or if the child is very uncomfortable and appears to have a bloated or full abdomen. Any AMT mini-one extension set fits any size AMT or MIC-KEY® gastrostomy tube.
Routine Changing Of Balloon Gastrostomy Tubes
The gastrostomy tube will need to be replaced when there is a malfunction, a poor fit or when it has been in for several months. Most parents are taught, in the hospital or office, how to change the gastrostomy tube and are comfortable changing the tube on their own. However, you can bring your child to the office or, in many cases, a home care nurse can be sent to your home to help you change the tube. A spare gastrostomy tube of the same size should be with your child at all times in case the balloon ruptures and replacement is required.
It is important to know the size of your child’s gastrostomy tube. It is printed in black letters on top of the gastrostomy tube. We recommend that you write down the size of your child’s tube on this document or someplace where you can find it when needed. This will help you when reordering supplies and talking with your child’s doctors and nurses.
pedsurg.ucsf.edu/conditions–procedures/gastrostomy-tubes.aspx
Homecare for Percutaneous Endoscopic Gastrostomy (PEG) Tube
Skin Care With the PEG Tube
Cleanse the area around the GT with water for the first two days after placement. After this, daily bathing with soap and water is all that is necessary. To clean the skin around the PEG tube, lift up the flap, inspect the area; wash the skin with soap and water and dry the skin completely. Most PEG tubes do not need a dressing. A small amount of drainage is normal. Turn the tube with each feeding to prevent skin irritation.
If the tube becomes too loose, spacers may be placed between the PEG and the skin to provide a better fit. If the tube gets too tight and there are spacers in place, these can be removed anytime, by your GI nurse or doctor.
After three months you may choose to replace the PEG with the same type of tube or you may change to a balloon type gastrostomy tube. Talk with your nurse or doctor about the best tube for your child. If the tube is working well and does not need to be changed at 3 months, it may stay in for up to one year.
PEG Tube Extension Sets
You will receive three types of extension sets. An extension set is a special tube that connects to the gastrostomy tube and allows formula, liquids and medicines to be given into the stomach. There is 1) a bolus set, 2) a right angle set and 3) a decompression tube. The bolus set is used for feedings given by gravity through a syringe. The right-angle set is used for slow or continuous feedings given by a pump. The decompression tube (which has a long tip which opens a valve at the base of the tube) allows air and formula to be drained from the stomach if needed. The decompression tube is used if a child has too much gas (which can’t be burped up) or if the child is very uncomfortable and appears to have a bloated or full abdomen. The nurses taking care of your child will show you how to attach and remove each extension tube.
PEG extension tubes must be the same size as the gastrostomy tube in order to fit. PEG tubes have two measurements, the diameter (width) measured in French (FR) size and the length measured in centimeters (CM). These numbers are printed on the inside flap of the PEG. The bolus set and the right angle set must be the same diameter (for example 14 Fr) as the PEG tube. The decompression tube must be the same diameter and the same length (for example 14 Fr and 1.7 cm) in order to fit. We recommend that you write down the size of your child’s tube on this document or someplace where you can find it when needed. This will help you when reordering supplies and talking with your child’s doctors and nurses. The office will also have a record of your child’s tube size.
pedsurg.ucsf.edu/conditions–procedures/gastrostomy-tubes.aspx
I found this thought it could show new Parents the view from a New Mum with a New Born Baby with a feeding tube.
Nasogastric tube (NG tube)
Don’t Panic your Hospital will teach you how to clear if it gets blocked, and always remember, your not the first to go through this, once you get the hang of it you feel right at home doing it in front of other’s, after all, said and done, your child needs feeding.
Here is a tip for you, Steve Wyles owner of this Website found this useful with his own daughter when she would pull out the tubes.
Stock Photo
Put mittens on your child’s hands to stop them from getting a hold of any tubes, they might otherwise pull on. This idea will help.


Word of warning, If you get the chance to carry a spare, it case Baby pulls one out, and Hospital doesn’t carry the size you need. The tube is taped to the child’s Face. Also your find your child will put this out.
Allow time for feed to go down this small tube.


Three ways of feeding this way, 3rd being via a Pump. This Site from a USA Hospital is a good thing to look through if your New to this.
www.childrensmn.org/Manuals/PFS/HomeCare/018701.pdf
A Facebook Group you might like to join
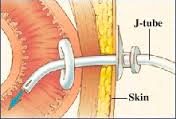
Jejunostomy is a surgical procedure in which a hole is made in the small intestine in order to insert a feeding tube. A patient may be given this operation if he has difficulty maintaining a healthy body weight by consuming food through the mouth. A jejunostomy tube (J-tube) may be used to introduce nutritious liquids and medicines to the body when the stomach is not fit for a feeding tube or in order to drain unwanted gases and liquids from the stomach.
NOTE, Children who suffer from BAD Reflux or poor gastric movement or who have had the op to lift the stomach up around the base of the esophagus, or can not have a gastrostomy tube inserted, then this might be the way forward
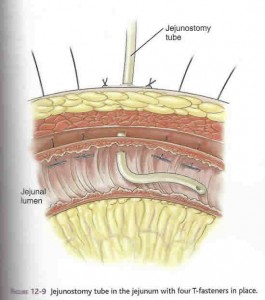
This procedure is typically recommended for patients who have a pancreatic disease, have difficulty emptying the stomach, or have a problem with the pulmonary aspiration of gastric contents, which occurs when the stomach contents are inhaled into the lungs. As an alternative to a gastronomy, in which the feeding tube is inserted into the stomach, a jejunostomy may also be used when the stomach needs to be kept strong for further surgeries.
The procedure is so named because the hole, or stoma, is made in the middle portion of the small intestine, or jejunum. The small intestine is a long tube that makes up part of the lower gastrointestinal tract, through which food moves to be digested. Sitting between the stomach and the large intestine, the small intestine is responsible for continuing to break down food that has already been partially digested in the stomach as well as absorbing the food’s nutrients. The remaining matter is then passed on to the large intestine, where the waste is prepared to be excreted. The jejunum segment of the small intestine is situated between the duodenum, which attaches to the stomach, and the ileum, which connects to the large intestine.
A Jejunostomy
A jejunostomy can either be performed as an open surgery, in which the patient is cut open to fully reveal the targeted tissue or as a laparoscopic procedure. In a laparoscopic operation, the patient will be anesthetized, and the surgeon will make tiny incisions in the belly through which a laparoscope and tools can be inserted. The laparoscope is an imaging device that allows medical professionals to see a real-time movie of the inside of the body without open surgery.
 Once the incisions have been made, the J-tube is pushed through the abdominal wall. If the belly were divided into four boxes or quadrants, the tube entrance would typically be made in the upper left quadrant. A small incision, usually of about 0.12 inches (3 mm), is then made in the jejunum and the tube is inserted so that its opening is in the lumen of the intestine. The lumen is the open space or canal in the center of the intestine. After removing the instruments and cleaning the incision sites, the patient should be ready to attach a feeding set and begin using the J-tube.
Once the incisions have been made, the J-tube is pushed through the abdominal wall. If the belly were divided into four boxes or quadrants, the tube entrance would typically be made in the upper left quadrant. A small incision, usually of about 0.12 inches (3 mm), is then made in the jejunum and the tube is inserted so that its opening is in the lumen of the intestine. The lumen is the open space or canal in the center of the intestine. After removing the instruments and cleaning the incision sites, the patient should be ready to attach a feeding set and begin using the J-tube.
Depending on the reason that the surgery is being performed, the patient may be able to return home and administer food and medicine independently. Nurses or doctors will brief the patient or Parents on how to use and maintain the feeding tube based on the particular case at hand. Generally, the tube and the skin around the tube should be cleaned daily with cotton pads or a washcloth and soapy water. The patient should be careful, however, not to get the area too wet when showering or taking a bath for the first four to six weeks. The tube should be flushed out with tepid water every six hours or after every feeding, as well as every time feeding is interrupted.
water every six hours or after every feeding, as well as every time feeding is interrupted.
If the J-tube site requires a dressing, this should also be changed on a daily basis. Patients should tell a healthcare professional if they experience redness, pain, swelling, or cracking of the skin surrounding the tube. The tube should also be secured to the body so as to prevent any pulling on the intestine. If the tube falls out, the opening should be covered with a fresh gauze pad and a medical professional should be notified.
You can buy these tube covers on the net or from groups.
http://www.practicalslpinfo.com/g-tube-removal-preparation-and-post-removal-instructions.html
Feeding tube removal is usually performed by a licensed health care professional, either a nurse or physician. Nasogastric feeding tubes are rigid plastic tubes that are inserted through the nose and passed down through the oesophagus to rest in the stomach. Duodenal feeding tubes are soft rubber tubes passed with the aid of a guide wire (which is later removed) into the stomach and then beyond it to the duodenum (the part of the small intestine just inches beyond the stomach). Percutaneous endoscopic gastrostomy, or “PEG” tubes, are inserted through the abdominal wall with the aid of an endoscope that has been passed from the mouth into the stomach. Nasogastric and duodenal feeding tubes are semi-permanent solutions that are left in place for days or weeks, whereas PEG tubes can be left in for years. The process of removal depends on the type of tube.
 Nasogastric and duodenal feeding tubes are generally secured to the nose using tape or some other method. The tape is removed; and with the patient sitting as upright as possible, gentle traction is placed on the tube to begin the withdrawal process from the stomach or the duodenum. Duodenal feeding tubes are typically smaller than hard plastic nasogastric tubes, and extra care is taken during removal as they can stretch and break. As the end of the tube gets near the top of the oesophagus, the nurse will likely pause and give the patient a moment to rest. When the patient is ready, the tube is pulled quickly through the oropharynx and out through the nose. This may stimulate the gag reflex, but only very temporarily until the tube is out.
Nasogastric and duodenal feeding tubes are generally secured to the nose using tape or some other method. The tape is removed; and with the patient sitting as upright as possible, gentle traction is placed on the tube to begin the withdrawal process from the stomach or the duodenum. Duodenal feeding tubes are typically smaller than hard plastic nasogastric tubes, and extra care is taken during removal as they can stretch and break. As the end of the tube gets near the top of the oesophagus, the nurse will likely pause and give the patient a moment to rest. When the patient is ready, the tube is pulled quickly through the oropharynx and out through the nose. This may stimulate the gag reflex, but only very temporarily until the tube is out.
Percutaneous feeding tubes are generally removed by a gastroenterologist or general surgeon. Removal typically involves deflating a balloon on the far end of the tube and withdrawing the tube through the abdominal wall to the outside. Some PEG tubes have a “bumper” that prevents pulling the tube through to the outside, in which case the tube is cut from the inside during an endoscopic procedure and removed through the mouth. In most cases, the external PEG openings are small and heal without formal intervention, but larger openings may need to be closed with sutures.
http://www.livestrong.com/article/71245-feeding-tube-removed/
Removing the Tube
If and when the doctor decides that your child is able to take in enough nutrition by mouth, the G-tube or button will be removed. Removal takes only minutes and is usually done in the office by the doctor or nurse.
Once the button or G-tube is out, a small hole will remain. It will need to be kept clean and covered with gauze until it closes on its own. In some cases, surgery is necessary to close the hole. Either way, the scar that remains will be small.
http://kidshealth.org/en/parents/gastrostomy.html
you-tube video of a Child having G-Tube Removed
Tube Removal: Cautions and Complications
From the Parent
I had to write this. My goal isn’t to scare parents who have kids getting their tubes removed. It’s just a warning to be cautious.
Getting a feeding tube removed is supposed to be a time for celebration. We waited four long years for my son Spencer to be tube free. We had his feeding tube removed on March 6th, 2014, in the clinic with his GI doctor. In theory, the stoma was supposed to close on its own, or leak a tiny bit and need surgical closure a couple weeks later. However, with Spencer, nothing ever goes as planned.
http://complexchild.org/articles/2015-articles/february/tube-removal/
No-tube
Has your child become dependent on the feeding tube?
We are focused on teaching children to learn how to eat whether they are suffering from tube dependency or other early eating behavior disorders. Our highly-specialized team is comprised of the most senior experts in tube weaning and early eating disorders with more than 30 years of clinical experience. Members of our team are based around the world enabling us to wean children off the feeding tube beyond language barriers.
Tube dependency is a rare and severe condition where a child becomes dependent on a feeding tube for nutrition even when he or she is capable of learning how to eat.
The negative side effects of tube dependency can become overwhelming and have a dramatic effect on both the child and the family.
Tube dependency can negatively impact a child’s growth, health, and further development.
Studies estimate that one of every 20 children who receive temporary feeding tubes becomes tube dependent.