chd plus other issues ea-tef & tof-oa
Other Health issues that might be linked
The resources on this site should not be used as a substitute for professional medical care or advice.
Congenital heart disease CHD
Other Health issues that might be linked
The resources on this site should not be used as a substitute for professional medical care or advice.
Congenital heart disease CHD
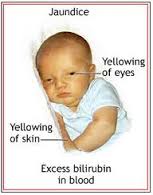 For most babies, this is a temporary, harmless condition that goes away on its own or with mild treatment. But in rare cases, it’s very serious, so it’s important to keep an eye on it. High levels of a pigment in the blood called bilirubin to cause the skin to look yellow. Everyone’s blood contains bilirubin. Bilirubin is one of the byproducts created when old red blood cells break down. During pregnancy, the mother’s liver eliminates bilirubin for her baby. After birth, it takes a while for the baby’s liver to start doing the job. The result: Pigment builds up in the baby’s blood and his skin takes on the yellowish cast of jaundice.
For most babies, this is a temporary, harmless condition that goes away on its own or with mild treatment. But in rare cases, it’s very serious, so it’s important to keep an eye on it. High levels of a pigment in the blood called bilirubin to cause the skin to look yellow. Everyone’s blood contains bilirubin. Bilirubin is one of the byproducts created when old red blood cells break down. During pregnancy, the mother’s liver eliminates bilirubin for her baby. After birth, it takes a while for the baby’s liver to start doing the job. The result: Pigment builds up in the baby’s blood and his skin takes on the yellowish cast of jaundice.
This type of jaundice, called physiologic jaundice, usually appears on a baby’s second or third day of life and disappears on its own within two weeks.
More info here www.babycenter.com/0_jaundice_89.bc
Biliary atresia
Bile is an important fluid produced by your child’s liver and stored in her gallbladder. In a healthy system, it flows through a tube called the common bile duct to the small intestine, where it helps to digest food. If your child has biliary atresia, her common bile duct is blocked or damaged, so that it’s impossible for bile to flow through it, just as it’s hard for water to pass through a clogged pipe. This is called “cholestasis,” or poor bile flow, and quickly leads to malnutrition and liver damage.
www.niddk.nih.gov/health-information/health-topics/liver-disease/biliary-atresia/Pages/facts.aspx
.
Known as HLHS
In hypoplastic left heart syndrome, the left side of the heart – the part that pumps oxygenated blood to the rest of the body – is underdeveloped. Its two chambers called the left atrium and the left ventricle, and their valves may be tiny, blocking the flow of oxygenated blood from the lungs.
The heart consists of four chambers: the two upper chambers called atria, where blood enters the heart, and the two lower chambers, called ventricles, where blood is pumped out of the heart. The flow between the chambers is controlled by a set of valves that act as one – Normally blood is pumped from the right side of the heart through the pulmonary valve and the pulmonary artery to the lungs, where the blood is filled with oxygen. From the lungs, the blood travels back down to the left atrium and left ventricle. The newly oxygenated blood then is pumped through another big blood vessel called the aorta to the rest of the body.
Babies with hypoplastic left heart syndrome may seem healthy at birth because the patent ductus arteriosus (PDA) is still open. The PDA is a blood vessel that connects the pulmonary artery to the aorta, allowing blood to continue circulating directly into the aorta and out to the rest of the body, bypassing the lungs and the defective left side of the heart. Once the PDA closes a few days after birth, blood flows to the lungs and then to the left side of the heart, where it is blocked and can’t circulate through the rest of the body.
Without treatment, babies afflicted with hypoplastic left heart syndrome can die within the first days or weeks of life. Treatment consists of a heart transplant or a series of operations to restore the function of the left side of the heart. Intravenous medication can keep the PDA open until surgery can be performed, but is not a permanent treatment.
http://www.pediatricct.surgery.ucsf.edu/conditions–procedures/hypoplastic-left-heart-syndrome.aspx
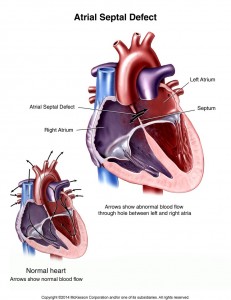
As a baby develops during pregnancy, there are normally several openings in the wall dividing the upper chambers of the heart (atria). These usually close during pregnancy or shortly after birth.
If one of these openings does not close, a hole is left, and it is called an atrial septal defect. The hole increases the amount of blood that flows through the lungs and over time, it may cause damage to the blood vessels in the lungs. Damage to the blood vessels in the lungs may cause problems in adulthood, such as high blood pressure in the lungs and heart failure. Other problems may include abnormal heartbeat and increased risk of stroke. Hypoplastic left heart syndrome (HLHS) is a birth defect that affects normal blood flow through the heart. As the baby develops during pregnancy, the left side of the heart does not form correctly. Hypoplastic left heart syndrome is one type of congenital heart defect. Congenital means present at birth.
With good Photos
http://www.cdc.gov/ncbddd/heartdefects/hlhs.html
https://youtu.be/oQlN6MfeX50
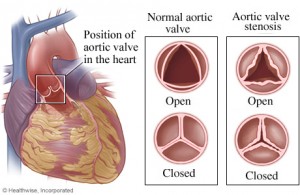
Aortic valve stenosis is an uncommon and serious type of congenital heart defect. It accounts for around 5% of cases of congenital heart disease.
In aortic valve stenosis, the aortic valve that controls the flow of blood out of the main pumping chamber of the heart (the left ventricle) to the body’s main artery (the aorta) is narrowed. This affects the flow of oxygen-rich blood away from the heart, towards the rest of the body, and may result in the left ventricle muscle thickening because the pump has to work harder.
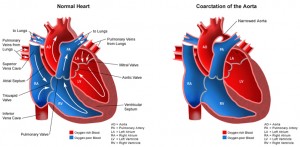
Coarctation of the aorta (CoA) is where the main artery (the aorta) has a narrowing, which means that less blood can flow through it.
CoA accounts for around 10% of cases of congenital heart disease. It can occur by itself or in combination with other types of heart defects – most commonly a ventricular septal defect or a type of defect known as a patent ductus arteriosus (see below).
In around half of all cases, the narrowing can be severe and will require treatment shortly after birth.
https://youtu.be/Ifkz76tQIKk
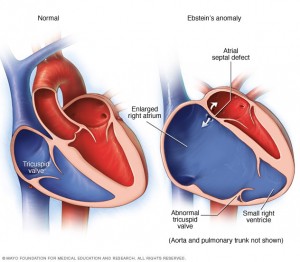
Ebstein’s anomaly can occur on its own, but it often occurs with an atrial septal defect (see below). It’s estimated that Ebstein’s anomaly accounts for less than 1% of congenital heart disease cases
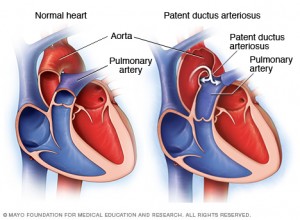
Patent ductus arteriosus (PDA) is a rare type of congenital heart disease, affecting around 5 in every 100,000 babies.
As a baby develops in the womb, a blood vessel called the ductus arteriosus connects the pulmonary artery directly to the aorta. The ductus arteriosus diverts blood away from the lung (which isn’t working normally before birth) to the aorta.
A patent ductus arteriosus is where this connection doesn’t close after birth as it’s supposed to. This means that extra blood is pumped into the lungs, forcing the heart and lungs to work harder.
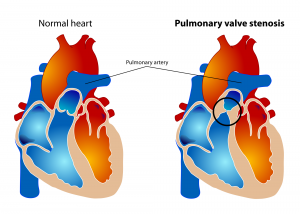
Pulmonary valve stenosis is a defect where the pulmonary valve, which controls the flow of blood out of the right heart pumping chamber (the right ventricle) to the lungs, is narrower than normal. This means the right heart pump has to work harder to push blood through the narrowed valve to get to the lungs.
Pulmonary valve stenosis accounts for around 10% of cases of congenital heart disease.
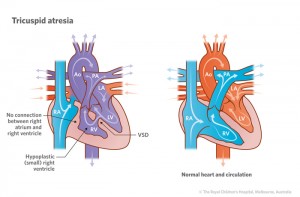
Tricuspid atresia is where the tricuspid heart valve hasn’t formed properly. The tricuspid valve separates the right-sided collecting chamber (atrium) and pumping chamber (ventricle). As there’s no blood flow into the right pumping chamber, the pump doesn’t develop and is too small.
It’s estimated that 10 babies in every 100,000 are affected by tricuspid atresia.
https://youtu.be/U4lOrV10QJ8
An atrial septal defect (ASD) is where there’s a hole between the two collecting chambers of the heart (the left and right atria). It’s a common type of congenital heart defect that affects about 2 in every 1,000 babies.
When there’s an ASD, extra blood flows through the defect into the right side of the heart, causing it to stretch and enlarge.
https://youtu.be/vz9nLV0Zvjk
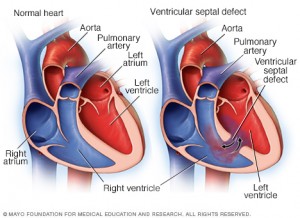
This means that extra blood flows through the hole from the left to the right ventricle, due to the pressure difference between them. The extra blood goes to the lungs, causing high pressure in the lungs and a stretch on the left-sided pumping chamber. Small holes often eventually close by themselves, but larger holes need to be closed using surgery.
A ventricular septal defect (VSD) is also a common form of congenital heart disease, affecting around 2 in every 1,000 babies. It occurs when there’s a hole between the 2 pumping chambers of the heart (the left and right ventricles).
This means that extra blood flows through the hole from the left to the right ventricle, due to the pressure difference between them. The extra blood goes to the lungs, causing high pressure in the lungs and a stretch on the left-sided pumping chamber. Small holes often eventually close by themselves, but larger holes need to be closed using surgery.
https://youtu.be/solK8GZupzw
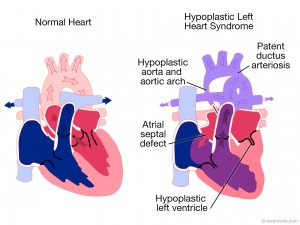
Hypoplastic left heart syndrome (HLHS) is a rare type of congenital heart disease, where the left side of the heart doesn’t develop properly and is too small. This results in not enough oxygenated blood getting through to the body.
Tetralogy of Fallot is a combination of several defects, affecting about 3 in every 10,000 babies.
The defects making up tetralogy of Fallot are:
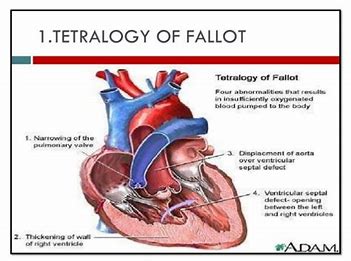
Click Blue Writing.
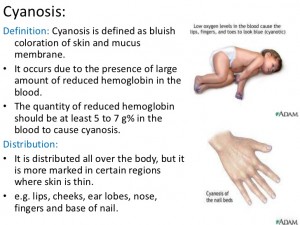
As a result of this combination of defects, oxygenated and non-oxygenated blood mixes, causing the overall amount of oxygen in the blood to be lower than normal. This may cause the baby to appear blue (known as cyanosis) at times.
https://www.uptodate.com/contents/overview-of-cyanosis-in-the-newborn#!
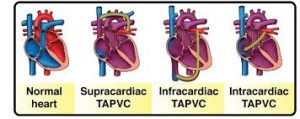 TAPVC occurs when the four veins that take oxygenated blood from the lungs to the left side of the heart aren’t connected in the normal way. Instead, they connect to the right side of the heart.
TAPVC occurs when the four veins that take oxygenated blood from the lungs to the left side of the heart aren’t connected in the normal way. Instead, they connect to the right side of the heart.
Sometimes, only some of the four veins are connected abnormally, which is known as partial anomalous pulmonary venous connection and may be associated with an atrial septal defect. More rarely, the veins are also narrowed, which can be fatal within a month after birth.
TAPVC is an uncommon type of congenital heart disease, affecting around 7 in every 100,000 babies.
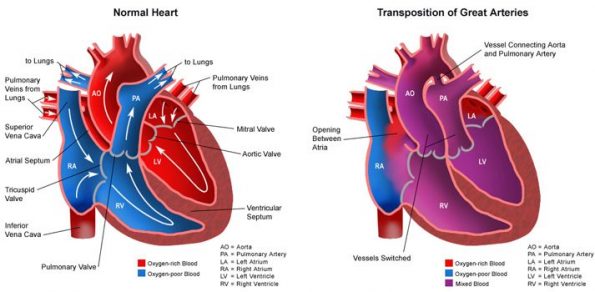
It’s where the pulmonary artery (lung artery) and main body artery (the aorta) are “swapped over” and are connected to the wrong pumping chamber. This leads to blood that’s low in oxygen being pumped around the body.
https://youtu.be/FGPEua3iBVY
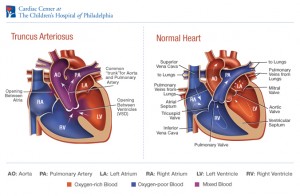
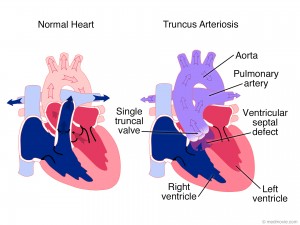 Truncus arteriosus is an uncommon type of congenital heart disease, affecting around 5 in every 100,000 babies. It’s where the two main arteries (pulmonary artery and aorta) don’t develop properly and remain as a single vessel. This results in too much blood flowing to the lungs which, over time, can cause breathing difficulties and damage the blood vessels inside the lungs.
Truncus arteriosus is an uncommon type of congenital heart disease, affecting around 5 in every 100,000 babies. It’s where the two main arteries (pulmonary artery and aorta) don’t develop properly and remain as a single vessel. This results in too much blood flowing to the lungs which, over time, can cause breathing difficulties and damage the blood vessels inside the lungs.
Truncus arteriosus is usually fatal within a year of birth if it isn’t treated.
https://youtu.be/U4lOrV10QJ8
What is a Congenital Heart Defect (CHD)?
A CHD means a child is born with an abnormally structured heart and/or large vessels. Such hearts may have incomplete or missing parts, maybe put together the wrong way, may have holes between chamber partitions or may have narrow or leaky valves or narrow vessels.
There are many types of congenital heart defects, ranging from those that pose a relatively small threat to the health of the child to those that require immediate surgery. Many types of CHDs and the surgical procedures your physician may recommend correcting the condition can be found in the Children’s Heart Foundation’s parent resource book.
http://www.childrensheartfoundation.org/research/what-is-a-chd
Facts about Critical Congenital Heart Defects
About 1 in every 4 babies born with a heart defect has a critical congenital heart defect (critical CHD, also known as critical congenital heart disease)Babies with a critical CHD need surgery or other procedures in the first year of life.
http://www.cdc.gov/ncbddd/heartdefects/cchd-facts.html
Specific Congenital Heart Defects
http://www.cdc.gov/ncbddd/heartdefects/specificdefects.html
Congenital heart disease is a general term for a range of birth defects that affect the normal workings of the heart.
The term “congenital” means the condition is present at birth. Congenital heart disease is one of the most common types of birth defect. In most cases, no obvious cause of congenital heart disease is identified. However, some things are known to increase the risk of the condition, including: WATCH A VIDEO ON THIS LINK
http://www.nhs.uk/conditions/Congenital-heart-disease/Pages/Introduction.aspx
Critical Congenital Heart Disease (CCHD)
Critical congenital heart disease (CCHD) represents a group of heart defects that cause serious, life-threatening symptoms and requires intervention within the first days or first year of life. CCHD is often treatable if detected early. It can encompass abnormalities in the rhythm of the heart, as well as a wide array of structural heart problems. These problems can range from mild (never requiring cardiac surgery), to severe (requiring multiple different stages of open heart surgeries). CCHD can involve abnormal or absent chambers, holes in the heart, abnormal connections in the heart, and abnormalities in the function or squeeze of the heart. Most congenital heart conditions affect patients from childhood through adulthood.
Some babies affected with CCHD can look and act healthy at first, but within hours or days after birth, they can have serious complications. Pulse oximetry newborn screening is a non-invasive test that measures how much oxygen is in the blood and can help to identify babies that may be affected with CCHD before they leave the newborn nursery. If detected early, infants affected with CCHD can often be treated and lead longer healthier lives. (USA)
http://www.babysfirsttest.org/newborn-screening/conditions/critical-congenital-heart-disease-cchd
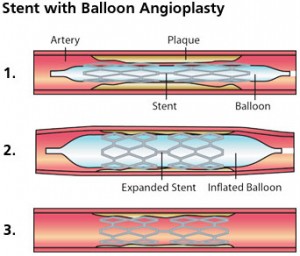
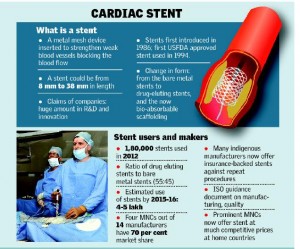
What is a Stent?
A stent is a tiny wire mesh tube. It props open an artery and is left there permanently. When a coronary artery (an artery feeding
the heart muscle) is narrowed by a buildup of fatty deposits called plaque, it can reduce blood flow. If blood flow is reduced
to the heart muscle, chest pain can result. If a clot forms and completely blocks the blood flow to part of the heart muscle, a heart attack results.
http://www.heart.org/idc/groups/heart-public/@wcm/@hcm/documents/downloadable/ucm_300452.pdf

This is truly outstanding
This animation shows how the novel UV-light enabled catheter can be directed non-invasively through a vein to reach a defect, or hole, in the heart. There, the catheter is pulled back to reveal a small device that uses small expanding balloons to seal off the hole in the tissue. The balloons deploy biodegradable adhesive patches which are cured within seconds by UV light emitted from the device. Then, the device and catheter are gently extracted, leaving the patch in a place where it supports tissue regrowth before it biodegrades naturally. Credit: Boston Children’s Hospital
Pedro del Nido, M.D., Chief of Cardiac Surgery at Boston Children’s and contributing author on the study, says the device represents a radical change in the way these kinds of cardiac defects are repaired. “In addition to avoiding open heart surgery, this method avoids suturing into the heart tissue, because we’re just gluing something to it.”
Fixing holes in the heart without invasive surgery.
Ultraviolet light equipped catheter | Boston Children’s Hospital – Boston Children’s Hospital
The non-invasive device, after being directed through a vein to the defect or hole in the heart, uses balloon technology to apply pressure and place the biodegradable patch over the defect. Then, as depicted in this digital rendering, UV light is emitted from the device and reflected inside the balloon, curing the patch. Afterward’s, the device will be gently removed leaving the patch adhered in place.
“The way the glue works in the face of blood is revolutionary. We don’t have to stop the heart,” says del Nido. “This will enable a wide range of cardiac procedures in the future.” By Erin Horan, Boston Children’s Hospital Communications.
(BOSTON) — Researchers from Boston Children’s Hospital, the Wyss Institute for Biologically Inspired Engineering at Harvard University, the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS), and the Karp Lab at Brigham and Women’s Hospital have jointly designed a specialized catheter for fixing holes in the heart using a biodegradable adhesive and patch.
Bringing HOPE to Parent’s, from the work by these outstanding dedicated Doctor’s and their teams, we thank you.
Watch this Video, this is what these Guy’s are working towards for making our life’s that little bit better. This Video is amazing.
http://www.youtube.com/user/wyssinstitute
Leah Burrows
Science and Technology Communications Officer
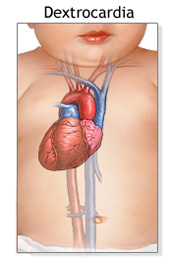 Dextrocardia is a rare condition in which, instead of being on the left side of your chest, your heart is located in the right side. Dextrocardia is congenital, meaning that you are born with this abnormality. Less than one percent of the general population is born with dextrocardia, according to the Texas Heart Institute Journal.
Dextrocardia is a rare condition in which, instead of being on the left side of your chest, your heart is located in the right side. Dextrocardia is congenital, meaning that you are born with this abnormality. Less than one percent of the general population is born with dextrocardia, according to the Texas Heart Institute Journal.
You may have dextrocardia and have a completely healthy heart. This is called “isolated dextrocardia.” People with isolated dextrocardia are sometimes affected by a condition called “situs inversus.” Situs inversus is a situation in which your liver, spleen, or other organs are also located on the opposite side of your body. Some people with dextrocardia suffer from other heart and organ problems related to their unique anatomy. Surgery may be required to correct complications with the lungs, heart, or digestive system in these cases.
Causes of Dextrocardia
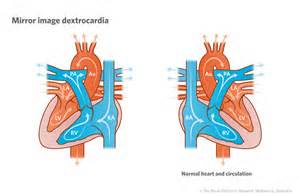 The cause of dextrocardia is unknown. The heart may form in the right side of the chest during fetal development and function normally. This is usually the case when the heart is a “mirror image” of a normal heart. In other words, the heart’s ventricles, arteries, and other structures are all arranged in a mirror image of normal heart structures.
The cause of dextrocardia is unknown. The heart may form in the right side of the chest during fetal development and function normally. This is usually the case when the heart is a “mirror image” of a normal heart. In other words, the heart’s ventricles, arteries, and other structures are all arranged in a mirror image of normal heart structures.
Sometimes, the heart develops on the opposite side of the body because other anatomical problems exist. Defects in the lungs, abdomen, or chest can cause the heart to develop on the right side of the body. You are more likely to have other heart defects and problems with other vital organs in this case. Multi-organ defects are referred to as “heterotaxy syndrome.”
For more info about Heterotaxy Syndrome
CLICK ON THIS LINK www.heterotaxy.org/pages/what_is_heterotaxy.aspx
Isolated dextrocardia usually causes no symptoms. The condition is usually found when an X-ray or magnetic resonance imaging (MRI) of the chest shows the location of the heart on the right side of the chest.
However, some people with isolated dextrocardia have an increased risk of lung infections, sinus infections, or pneumonia. According to the National Institutes of Health, reduced function of the cilia in the lungs can accompany isolated dextrocardia. Cilia are very fine hairs that filter the air you breathe. When the cilia are unable to filter out all viruses and germs, you may get sick more often.
Dextrocardia that affects heart function can cause a variety of symptoms, including:
These symptoms are consistent with defects in the ventricles of the heart. Lack of oxygen reaching the heart can make you tired and prevent you from growing normally. Abnormalities that affect the liver can cause jaundice, a yellowing of the skin and eyes. Some children with dextrocardia also have holes in the septum of the heart. The septum is the divider between the left and right heart chambers. Septal defects can cause problems in the electrical system of the heart, and the heart rhythm can become irregular.
Some babies with dextrocardia are also born without a spleen. The spleen is a major part of the immune system. Without a spleen, there is a higher risk of developing infections throughout the body.
Treating Dextrocardia
Dextrocardia must be treated if the abnormality prevents vital organs from functioning properly. Pacemakers and surgery to repair septal defects can help the heart work normally.
Antibiotic medications will be prescribed to prevent infection if the spleen is missing or not working properly. Long-term antibiotics may be used to fight off respiratory illness. Although medications reduce the risk of infection, individuals with dextrocardia may still suffer from more infections than the average person.
You will also be watched for abdominal obstruction. Abdominal obstruction, also called bowel or intestinal obstruction, prevents waste from exiting the body. The placement of your heart on the right side of the body makes blockages in your digestive system more likely. This is because dextrocardia can sometimes result in a condition called intestinal malrotation, in which the gut does not correctly develop.
Intestinal obstruction is dangerous and can be fatal if left untreated. Surgery is required to correct obstructions.
Long-Term Outlook
People with isolated dextrocardia are likely to live a normal life. Those with more complicated cases may face health problems throughout their lives. Even with surgical repair of heart defects, frequent illness is to be expected. Males with cilia problems may be infertile due to the resulting decreased ability of the sperm cells to propel themselves forward and fertilize the female egg cell.
www.healthline.com/health/dextrocardia#Overview1
Synonyms of Dextrocardia with Situs Inversus
http://rarediseases.org/rare-diseases/dextrocardia-with-situs-inversus/
http://radiopaedia.org/articles/situs-inversus
http://medical-dictionary.thefreedictionary.com/situs+inversus
http://health.howstuffworks.com/human-body/parts/reversal-of-organ1.htm
Responsive website designed & developed by
![]()