Chris is an ADULT TEF from the USA
Esophageal Atresia from Chris’ Corner
Being an adult with long gap esophageal atresia (EA) is a challenge. I am 45 years old and I am sitting in a hospital where most doctors do not know how to help me. I had my first surgery when I was two days old. My name on the first operative report read “Baby Boy” with my last name. That was in 1969 when the mortality rate for EA was 90%. Most infants died unexplained as most parents did not perform autopsies on their babies. It was simply explained as crib death like all other unexplained infant deaths.
When I had my colonic interposition, it was first put in in 1970. From what I’ve learned it was a staged procedure. The doctors back then didn’t know a lot. They put a very long piece of the colon between my throat and stomach. I was born with true long gap esophageal atresia. The true definition of EA is “born with the absence of an esophagus”. Having no esophagus, and my stomach was flat, my stomach had to be inflated before my two operations for connections at the proximal (top) and distal (bottom) ends could be connected. When the piece of the colon was introduced, the medical team anticipated me to grow as tall as my father, who is just over 6 feet tall. I didn’t quite make it. I am only 5’ 8” in height. I didn’t learn how long it actually was until 2012 when I had to have a surgical revision due to major difficulties. The piece of the colon in my chest did a job it should never have had to do for over forty years. The conduit I learned was 60 cm in length. A normal human esophagus is only 26 cm. Since the segment is too long it is now twisted and tortured. It has grown fist-sized diverticula “pockets”, causing food debris to get stuck and forms what I learned to be known as “bezoars”, which simply put, is a giant food ball.
The bezoar issue was discovered in 2011 after I was hospitalized again for unexplained pain in my chest that wasn’t heart (cardio) or lung (pulmonary) related. My gastroenterologist did an endoscopy and reported his findings to my wife in the waiting room following the egd. The doctor drew a picture of my unique anatomy. Since then my wife has searched the world for answers on how to get help for me and my condition. I imagine she gets tired of asking doctors for help and they all scratch their heads in puzzlement as to what’s wrong with me and don’t know what to do for me. She spends every moment of her spare time
researching new EA studies, modern treatment options, searching the world via the internet & reaching out to whoever will listen. She’s desperately trying to get together a team to study EA & it’s long-term complications, and what can be done to effectuate treatment of Adult EA. Her goal is to lessen my suffering and in the process open doors to all the children born with EA, who are going to grow up and be in the same boat I am. Which, by the way, is a very frustrating and shitty place to be. Imagine knowing there’s something wrong with you, but no-one knows how to fix it.
It’s usually a good 10-12 hours for each ER visit starting with the fight at triage with getting in the door and explaining chest pain that’s not a heart attack. I am usually in too much pain at this point to speak and like to rely on my wife, who is also more knowledgeable about my condition than I am, to speak for me. Most don’t listen. They think that they know how to help and the simplest solution often is ignored…Listen to the patient. Ask don’t tell. If an “in pain” patient asks you to let their advocate speak for them, let them. The more resistance that occurs, the more stressful for the already distressed patient.
 This proceeds to a long wait in an ER stall before a nurse checks on you. Then it’s another long while before a doctor sees you. Not to mention all kinds of tests in between. Then, if you’re fortunate, the doctor listens, understands and is helpful getting you relief from the pain. If not, you suffer, in public, for hours, unmercifully.
This proceeds to a long wait in an ER stall before a nurse checks on you. Then it’s another long while before a doctor sees you. Not to mention all kinds of tests in between. Then, if you’re fortunate, the doctor listens, understands and is helpful getting you relief from the pain. If not, you suffer, in public, for hours, unmercifully.
After being admitted to the hospital & settled in my room it’s now the next day. I seem to do Ok with the daytime nurses when doctors are around, and help is readily available. It’s the night time when I run into trouble. I called the nurse on duty for pain meds. I have a lot of pain in my colonic interposition, the kind of pain that morphine only takes the edge off, it doesn’t completely go away. The nurse came & gave me the dose of medicine in my IV line. The pain didn’t go away. It kept increasing. I called the nurse again, not only was I in pain with my GI issues, my IV port in my wrist was hurting and swollen. She came and looked at it and said “it’s fine” and left. I called the nurse again, and she brought another tech(nurse’s aide) with her & they both looked at me & said “you’re fine” & left the room. I am mad now, but what can I do? My pain is worse, I called for help and there’s no-one to help me. I don’t want to call my wife at 3 am and wake her up. She stayed with me until 10 pm, then went home to take care of our 16 yr. old, and our two grandsons aged 3 & 4. I laid there for 4 hours, hurting more and more and more. Finally, a new shift came on at 7 am and came to check on me at 7:30 am. I was in so much pain, I was doubled over & could hardly talk. Thank goodness this day nurse knew what to do and saw how much trouble I was in. She summoned a team to put in a “central Line IV” also known as a Pick-Line where an ultrasound was used to find a big enough vein in my arm under my armpit with an 18 gauge needle to ensure proper flow of desperately needed pain medication and nutrients via a drip. Why am I even here at a hospital if they can’t help me? Isn’t a nurse supposed to care for me? When my wife was here last night, she spoke with the doctor. She asked the doctor what happened if the medicine I was on was not strong enough? He advised her & me that if I exceeded what was prescribed it was OK to page him or any doctor on call and orders were written to prescribe me what I needed. If a doctor orders care, and a nurse ignores those instructions, and a patient suffers, what other recourse do I have laying there, hooked up to machines and needles and helpless??
When my wife called me at 8 am, I couldn’t even talk. I was barely able to tell her what was wrong. She dropped the kids at their grandmother’s and rushed to the hospital and had a long talk with the charge nurse and the nursing manager. Believe me when I tell you that you would not like to be on the receiving end of that conversation. It’s unacceptable to let a patient suffer like that. She gets a little feisty when it comes to caring for someone she loves. If it weren’t for her I would not understand my condition as I do today. She fought for 5 years to get all my medical records. Read every single word of what was done to me and for me. I got a medical dictionary and carries it around in her purse along with my condition notes and pictures to advocate for me.
I am in the hospital again. This makes twice within a month. I made it through triage, made it to the ER “stall”, just had a dose of pain meds, more x-rays & got lucky this round with a few caring doctors trying to help me. The GI team came in and I am being admitted, again.
Thank goodness, my parents, the nurses and the doctors that were present during my first two days of life recognized something was wrong. From what I’ve been told, I didn’t have a
and nothing would go down. They tried sticking something down my throat and it didn’t get very far. After reading my infant hospital reports, I now have a greater understanding of what I went through. Although, I didn’t realize any of this until I was an adult.
Don’t get me wrong. I always knew something was wrong. I had to eat slower than everyone else. I always had to be careful of what I ate. If I ate too fast, food would get stuck and I would have to make myself throw up because it felt like someone was choking me. But I grew up, not wanting to be different. No matter how much I want to not be different, I am. My old body tells me more and more every day.
I didn’t have a lot of major issues as I kid. If I ate slow, I did great. If I ate too fast I’d have to make myself throw up. I always drink a lot of fluid when I eat too. I have a piece of the colon between my throat and my stomach, I don’t have the muscles in my throat that an esophagus has to squeeze food down. That process is called peristalsis. I have no peristalsis. I rely on gravity to get my food to my stomach. This worked for me until I became an adult.
As an adult, I didn’t know a lot about EA. I knew I had issues, but I knew how to manage and get by. I had a few major issues with pain and bleeding ulcers and was often misdiagnosed as having colitis, GERD, bleeding ulcers etcetera. I went to the emergency room a few times. They managed my pain, gave antibiotics and sent me home.
This continued into my thirties. This is when I met my wife Sue. We were married in 2006. I first was embarrassed to tell her about all my surgeries. I made up stories about my scars. I didn’t want her to think less of me. This was before I realized how much she cared about me and loved me. I eventually told her the truth. I had a bad accident shortly after we took our vows. We were married in December and on July 27th, I got hit by a train.
I was a passenger in a work truck, and the driver drove into the path of an oncoming train. The train struck the passenger side where I was sitting and pushed the truck 40 feet into a ditch. I had multiple injuries from head to toe, and am lucky to be alive. Most people do not meet a train, get hit and live. When I was in the hospital, my wife never left my side. I couldn’t walk or talk for a few days. She said when she arrived at the hospital, she was led to an empty emergency room stall. There was blood and broken glass everywhere, but not me. She told me that I had been wheeled to radiology for a CAT scan and x-rays. She followed the signs to radiology and found me behind a glass wall struggling and screaming for her. A little 4-foot tall doctor told her she couldn’t see me. What is the harm of a loved one reassuring a patient? She pushed past the doctor and help my hand for a few moments before the little doctor called security on her and a security guard escorted her out of radiology and into a waiting room. She told me about the kind security guard who prayed with her and told her that everything was going to be alright. It was then I got a second chance at life and became more honest about my condition. When I was incapacitated, there wasn’t a lot I could do for myself. My wife helped me through the hospital stay of two weeks, then helped me with my care as I couldn’t even walk. I progressed from a walker to a cane. After lots of physical therapy and care from my wife, I eventually recovered, walked again and began to look at things a lot differently.
After the train wreck, we moved to Maine to live with my wife’s family. About a year later I started having issues with my digestive system again. I would hurt a lot, with pain so bad, my wife would take me to the emergency room. This increased in frequency from once a year to about 4-5 times per year for the next few years. All kinds of doctors visited me and tried to figure out what was wrong with me. I have had so much radiation and barium I’m surprised I don’t glow.
I had the pleasure of being introduced to a very smart and caring gastroenterologist named Dr. Andreas Stefan. He happened to be the doctor on duty during hospitalization and performed an endoscopy on me. He discovered a giant food ball in me & is now what is known as a bezoar. It was a diverticula pocket filling up with what I ate. Instead of what I ate getting to my stomach, this pouch was beside the opening to my stomach and collected what was supposed to continue through my stomach and on to the intestines. Following the egd, Dr. Stefan met with my wife in the waiting room. He drew her a picture of what my anatomy looked like. He explained to her a lot about my condition, which she then explained to me. She usually gets to talk to the doctors performing the procedures as I am most times just
the mass was so large, the rest had to “pass” slowly and painfully over the next week in the hospital.
This is when my wife started her research on EA. I think she’s read every study, every procedure and everything there is to read about EA. What causes it, how it happens, what happens to repair the condition, what procedures were first done, how treatment has evolved from archaic colonic interpositions to modern colonic interpositions(both ileum & jejunal), fonduplications, Iver-Lewis techniques, the “Foker procedure”, stomach stretching & pulling, magnetic stretching, and I think a few that aren’t mentioned. You can ask my wife what’s in her library. I know a lot is done nowadays for children that never was available when I was born. The first-ever Esophageal Atresia Treatment Program was just started in 2012 by Dr. Russell Jennings. It was my wife’s research that found out about Dr. Jennings & what he was doing for EA as his program was starting. She reached out to Dr. Jennings and he was kind enough to look at my records. Unfortunately, I was just over the age of forty and the EAT Program is for pediatric patients (children). But, what happens when a child gets repaired, and supposedly “fixed” but not cured? What are the long-term complications? There is no adult treatment for Esophageal Atresia. What happens when you’re born with EA, get repaired, and grow up?
Dr. Jennings referred me to Dr. Raphael Bueno, then Assistant Chief of Thoracic Surgery. Dr. Bueno performed a surgical revision in June 2012 at Boston’s Brigham & Women’s Hospital. That surgery shortened my colonic interposition, tightened it, and revised my colo-gastric connection from the side of my stomach where it was, to a more centralized connection in the middle of my stomach. That was an 8-hour operation, and a two week stay in ICU. That surgery enabled me to go from being hospitalized 4-5 times per year, to go 18 months without an issue. But, eventually, the issues returned. Dr. Bueno explained that it was only a temporary solution.
In the meantime, we moved from New England to North Carolina and I am back to being treated at the University of North Carolina at Chapel Hill. This teaching hospital saved my life in 1972 when my first surgeries were leaking and bleeding at the anastomosis (attachments). They had the ability to repair me, and monitor me from toddler to a teenager.
Now I am in their hands again facing yet another major surgery. After years of surgical specialists’ consultations, gastroenterologist’s recommendations, radiological evidencing, the future only holds another major surgery for me. The colonic interposition I have now is failing. I am in the hospital again for the second time this month. I have an endoscopy scheduled for tomorrow morning to see if anything is different or still the same or worse.
I am now joining Steve Wyles and Bev Stark and their awareness for Esophageal Atresia campaign. If what I am going through can offer some sort of solution or learning experience for doctors today to help children growing up with EA, then what I am going through and about to go through is worth the effort. I pray that no-one walks in my shoes and that someday there will be a treatment for Adult Esophageal Atresia.


 I am 55 years old and have lived a relatively healthy adulthood but as a newborn I had TEF. I come from Detroit, Michigan born in 1962, I have 3 older siblings, back then both of my parents drank and smoked cigarettes ( I do not know if this had any cause and effect on my TEF) my mothers parents had just passed away while pregnant with me, I was told growing up that she had a mini-stroke during the pregnancy.
I am 55 years old and have lived a relatively healthy adulthood but as a newborn I had TEF. I come from Detroit, Michigan born in 1962, I have 3 older siblings, back then both of my parents drank and smoked cigarettes ( I do not know if this had any cause and effect on my TEF) my mothers parents had just passed away while pregnant with me, I was told growing up that she had a mini-stroke during the pregnancy.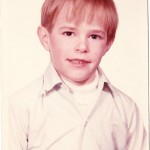 was picked on (bullied) for most of my school years, But most of my bullies became friends even through high school.
was picked on (bullied) for most of my school years, But most of my bullies became friends even through high school.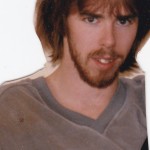 and started our own team.
and started our own team.
 I first met Claudia in 1988 when a “full grown” woman came to my clinic in Milwaukee carrying a large x-ray envelope with her. I was certainly baffled when I found out that she was not a mother of a patient but rather the patient herself. When I informed her that my practice was limited to the surgical care of infants and children, she countered by stating that although she was an adult, her problem is that of the very young. And sure enough, when I reviewed her films it was readily obvious that Claudia had recurrent TEF. I was especially amazed not only to find out that she was the first successfully repaired EA/TEF in the state of Wisconsin, but also that she, in essence, had symptoms of TEF all of her life. None of the family members nor the various medical doctors (from pediatricians to OB/GYN to internists) even thought to relate her chronic coughing (especially when drinking) and repeated chest infections to the possibility of recurrent TEF. From her story, I concluded that her recurrence happened early in the postoperative period (back in 1953) and that is one of the reasons she had to spend 9 months in the hospital and resort to the “best healer of all,” God, to see her through this dangerous time. And here she was, a mature woman, mother of two, who played tennis (and even smoked cigarettes!) who endured a “stormy” infancy and lifelong lung symptoms; who despite it all remained kind and mannered and to whom one had to speak straight to her face so that she could understand one’s speech. She, in other words, was irresistible and I promised her that I would correct her problem surgically.
I first met Claudia in 1988 when a “full grown” woman came to my clinic in Milwaukee carrying a large x-ray envelope with her. I was certainly baffled when I found out that she was not a mother of a patient but rather the patient herself. When I informed her that my practice was limited to the surgical care of infants and children, she countered by stating that although she was an adult, her problem is that of the very young. And sure enough, when I reviewed her films it was readily obvious that Claudia had recurrent TEF. I was especially amazed not only to find out that she was the first successfully repaired EA/TEF in the state of Wisconsin, but also that she, in essence, had symptoms of TEF all of her life. None of the family members nor the various medical doctors (from pediatricians to OB/GYN to internists) even thought to relate her chronic coughing (especially when drinking) and repeated chest infections to the possibility of recurrent TEF. From her story, I concluded that her recurrence happened early in the postoperative period (back in 1953) and that is one of the reasons she had to spend 9 months in the hospital and resort to the “best healer of all,” God, to see her through this dangerous time. And here she was, a mature woman, mother of two, who played tennis (and even smoked cigarettes!) who endured a “stormy” infancy and lifelong lung symptoms; who despite it all remained kind and mannered and to whom one had to speak straight to her face so that she could understand one’s speech. She, in other words, was irresistible and I promised her that I would correct her problem surgically. little inflammation around it – suggesting that the tracheoesophageal fistula — was, indeed, of longstanding. When we disconnected the trachea from the esophagus, we repaired the two side holes in them. In order to secure the repair and prevent re-recurrence of TEF, I “borrowed” adjacent tissue and imposed it between the two suture lines. She healed promptly. However, as you heard, her esophagus developed some scarring in the area for which occasional dilations were required. It was particularly interesting for me to talk to Claudia about her lifelong esophageal problem. Since all babies with EA/TEF have impaired motility of the esophagus, Claudia is (was) not an exception. She can describe a “bolus” (chunk) of food slowly descending down the esophagus with the “descending” discomfort it produces. Her post problem with “food getting stuck” in the esophagus is a most typical occurrence in our babies and most parents can agree to that. She soon learned to chew her food well, eat small pieces and drink frequently with her meals. No question these points are driven home frequently to all parents with EA/TEF babies. The message from Claudia for all of us to remember is not only the triumph of the spirit. Also, one need not to ignore symptoms but to pursue them with persistence and vigor. Claudia is lucky not to suffer the consequences of her chronic TEF, namely chronic, debilitating lung
little inflammation around it – suggesting that the tracheoesophageal fistula — was, indeed, of longstanding. When we disconnected the trachea from the esophagus, we repaired the two side holes in them. In order to secure the repair and prevent re-recurrence of TEF, I “borrowed” adjacent tissue and imposed it between the two suture lines. She healed promptly. However, as you heard, her esophagus developed some scarring in the area for which occasional dilations were required. It was particularly interesting for me to talk to Claudia about her lifelong esophageal problem. Since all babies with EA/TEF have impaired motility of the esophagus, Claudia is (was) not an exception. She can describe a “bolus” (chunk) of food slowly descending down the esophagus with the “descending” discomfort it produces. Her post problem with “food getting stuck” in the esophagus is a most typical occurrence in our babies and most parents can agree to that. She soon learned to chew her food well, eat small pieces and drink frequently with her meals. No question these points are driven home frequently to all parents with EA/TEF babies. The message from Claudia for all of us to remember is not only the triumph of the spirit. Also, one need not to ignore symptoms but to pursue them with persistence and vigor. Claudia is lucky not to suffer the consequences of her chronic TEF, namely chronic, debilitating lung



