Does Fish oil help fight off colds?
( Please ask your Doctors before giving omega fish oil or cod liver oil)
On a Personal Note
I (Steve Wyles) worked outside in all weathers, for 16 years and I took a high dose of omega 3, tablet, every day, and rarely got a bad standard cold. My own daughter has a very poor immune system, because of her rare condition, but she lives on a high-fat diet to fuel her brain etc and rarely gets a cold. I personally believe this has something to do with her high-fat diet
I cant say this will help your Children. But ask your Doctor’s you never know
Colds are no fun for anyone, but for newborns, any assault on their still-developing immune systems can be dangerous. But moms-to-be can reduce the risk that their little ones will get sick by taking fish oil supplements.
In a study published in Pediatrics, researchers at Emory University and in Mexico report that women taking 400 mg of docosahexaenoic acid (DHA), an omega-3 fatty acid found in fish oil, helped their one-month newborns to fight off more cold symptoms such as coughing, nasal congestion and runny noses than moms who took a placebo. The cold-fighting effect lasted for six months; by that time, the DHA-protected infants experienced about the same amount of cold symptoms as the babies whose mothers did not take DHA, but their symptoms didn’t last as long.
“I wouldn’t want to overplay the benefits, but the findings do suggest some benefits early in life,” says the study’s lead author Usha Ramakrishnan, a professor in the department of global health at Emory University School of Public Health. “This is one of the first studies to look at nutritional interventions during pregnancy and immune function of newborns later on.”
READ ON
http://healthland.time.com/2011/08/01/fish-oil-during-pregnancy-fights-colds-among-newborns/
.
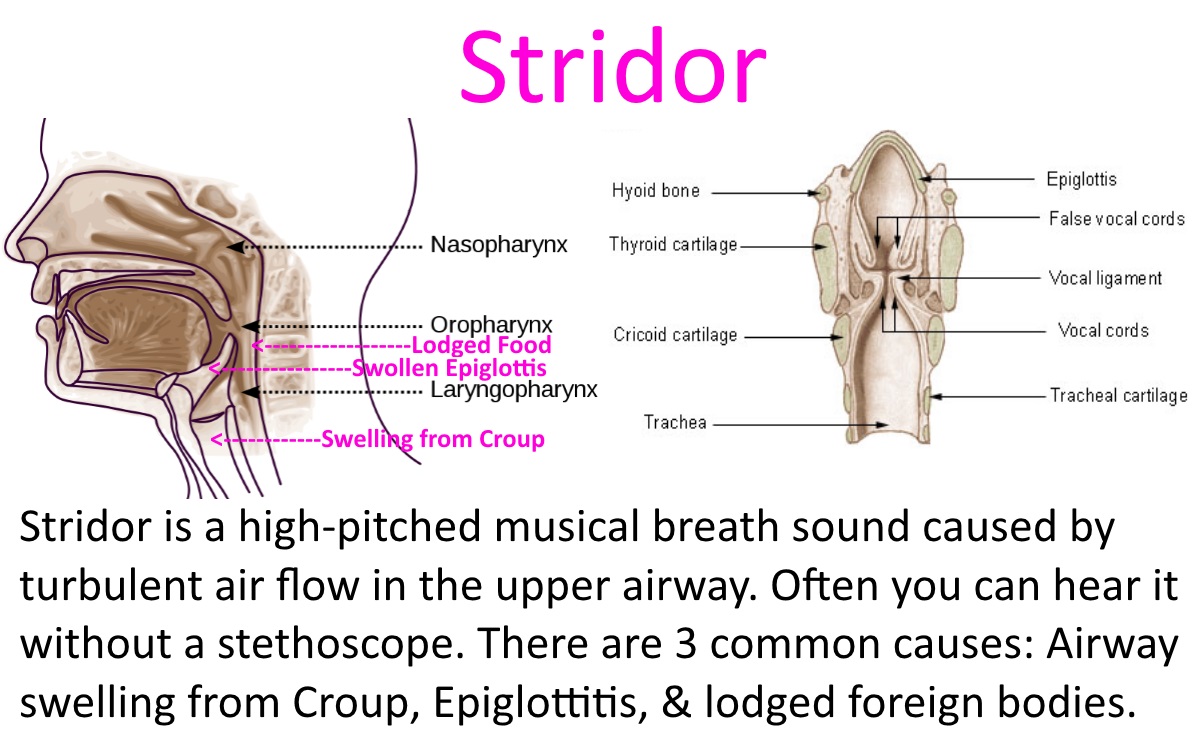
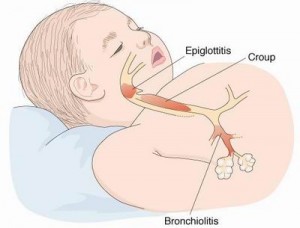
How to Use Cod Liver Oil to Fight Upper Respiratory Inflammation
Click on the underlined RED wording
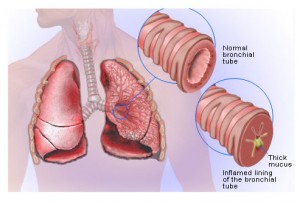
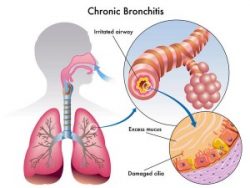
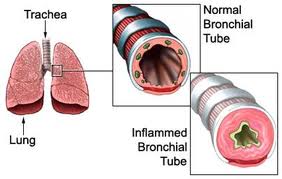
1. Fish oil relaxes tight air passages.
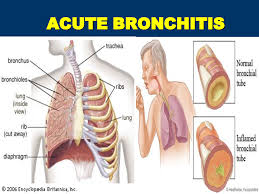
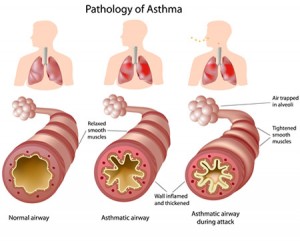
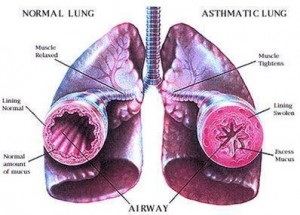
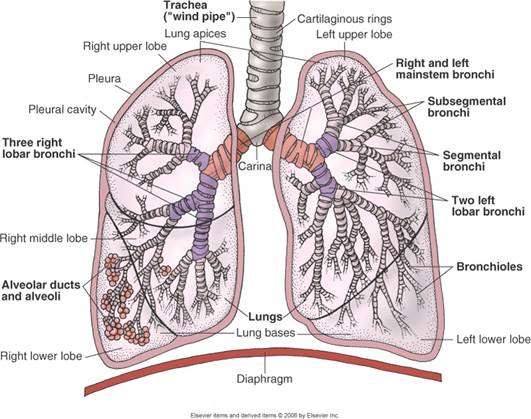
One of the first things you notice when you get a cold is a tingly sensation in your nostrils, and maybe in the back of your throat. This is quickly followed by irritation and a sensation of tightness. Exercise physiologists at Indiana University have found that taking fish oil relieves tight, constricted breathing passages just as effectively as a nose spray or, in some cases, as an inhaler.
These scientists also found that using both fish oil and a medication has no cumulative benefit in relieving upper respiratory airway constriction, and, of course, you need to be taking fish oil before you come down with the infection. That is, be sure to add fish oil to your supplement routine at the beginning of your colds, flu, or allergy season.
2. Fish oil relieves allergic inflammation.
While many of us ask ourselves the question of whether what we have is a cold or an allergy, the simple fact is, a lot of the time it’s both. Fish oil contains omega-3 essential fatty acids that relieve inflammation caused by allergies.
3. Cod liver oil corrects vitamin D deficiency.
One of the reasons we get colds when the weather gets cooler is that many kinds of rhinoviruses are activated by lower temperatures. Another of the reasons we get colds when the weather gets cooler is that we spend more time in confined spaces with other people who may be infected. And a third reason we get colds when the weather turns cooler is that the days are shorter and our bodies don’t make as much vitamin D.
But that doesn’t mean we need supplemental vitamin D all the time. And I’ll explain what this has to do with fish oil in a moment.
Researchers Dr. John Aloia and Dr. Melissa Li-Ng at the Winthrop University Hospital in Mineola, New York tracked patients who took no supplemental vitamin D, 800 IU of supplemental vitamin D daily, and 2000 IU of supplemental vitamin D daily throughout an entire year. They found that the participants in their study who took no supplemental vitamin D at all reported 25 days during the winter when they felt symptoms of colds or flu.
The researchers found that study participants who took 800 IU of vitamin D a day reported just 3 days during the winter when they felt colds or flu, and that those who took 2000 IU of vitamin D a day didn’t have any colds or flu days at all during winter months. Aloia and Li-Ng, however, did not just study the effects of vitamin D during the winter. They also tracked their patients during the spring, summer, and fall.
People who didn’t take any vitamin D at all tended to have a few “cold and flu days” during every season of the year. People who took 800 IU of vitamin D a day had just 1 or 2 days with symptoms during every 3-month period. People who took 2000 IU of vitamin D a day didn’t have any colds or flu during the winter, spring, or fall, but tended to have 1 or 2 days with symptoms in the summer.
This study suggests that vitamin D protects against colds and flu, but it may be possible to get too much as well as too little. I don’t recommend anyone take vitamin D for colds and flu prevention during the summer. Taking vitamin D during cool-weather seasons is enough.
But what does that have to do with fish oil?
Cod liver oil is a great source of both omega-3 essential fatty acids and vitamin D. It is an easy way to get both the omega-3’s that fight inflammation and the vitamin D that fights infection.
Fish oil typically does not contain vitamin D, and shark liver oil contains a lot of substances you just don’t want to take into your body. Cod liver oil, in capsules, is the easiest way to get both omega-3’s and vitamin D in a single dose, nine months of the year.
Nowadays, cod liver oil doesn’t taste bad. You can still buy a big bottle of liquid cod liver oil, and some companies, like Green Pasture, offer excellent prices for cod liver oil in bulk. Chances are, however, that you and your family would prefer cod liver oil capsules like those made by Nordic Naturals for use by the entire family throughout autumn, winter, and spring.
You’ll catch fewer colds outside the home, and there will be less sharing of colds and flu through the family, due to the generous provision of vitamin D. Just be sure to take enough cod liver oil to get 2,000 IU of vitamin D a day for adults, or 1,000 IU per day for children.
.
Kick Colds Fast With A Detox Bath.
If you want to be prepared for a new flu season, then I have an amazing tip for you: How To Kick Colds Fast With A Detox Bath.
After several years of learning about natural remedies, a good detox bath is one of my favorite ways of kicking a cold fast. Taking a detox bath will help your kids relax, clean their systems of toxins, and absorb wonderful minerals that will strengthen their immune systems.
After a full day of activities, your kids are feeling miserable because of a cold. They are cracky, congested, irritable and just a mess. How To Kick Colds Fast With a Detox Bath is the perfect way to make your kids feel better and relaxed when they are sick. In my experience, it really helps.
A few weeks ago, my 5-year-old son caught a cold. The same day he started to show cold symptoms, I made sure to give him a detox bath. He slept for 12 hours straight afterwards! He woke up the following morning feeling much better. This is when I realized I had to write a post about detox baths.
Your kids are exposed to a lot of toxins from pollution, household cleaners, and processed foods that are full of chemicals and additives. A detox bath with magnesium has the power to eliminate those toxins. So it is also a good idea to just give your kids a detox bath once a week, even if they are not sick to keep their immune systems strong and free of toxins.
I try to take a detox bath once a week too. It is so relaxing and I feel completely rested and energized the following day. If you want to learn all about detox baths and why you should take them, please see this wonderful article HERE. It explains in depth all the wonderful benefits of taking a detox bath.
Studies have shown that magnesium and sulfate are both readily absorbed through the skin, making Epsom salt baths an easy and ideal way to enjoy the associated health benefits. Magnesium plays a number of roles in the body including regulating the activity of over 325 enzymes, reducing inflammation, helping muscle and nerve function, and helping to prevent artery hardening. Sulfates help improve the absorption of nutrients, flush toxins, and help ease migraine headaches.
http://creativeandhealthyfunfood.com/how-to-kick-colds-fast-with-a-detox-bath/