Other Conditions that could be under the surface
Other Rare
items worth
looking at
So
‘Bridging
the
Gap’
of understanding
Other Rare
items worth
looking at
So
‘Bridging
the
Gap’
of understanding
Malabsorption is a condition in which your digestive system loses the ability to absorb certain nutrients. It can be caused by a variety of illnesses or can happen as a side effect of some types of medications and surgical procedures. Some forms of malabsorption, such as pernicious anemia, are unique to particular nutrients (in that case, a vitamin B-12 deficiency) while other malabsorption syndromes can be more general when you lose the ability to absorb several nutrients. Digestion is completed in the small intestine where enzymes released by the pancreas break those smaller pieces down into individual nutrients (both micro and macronutrients) that can be absorbed through the walls of the small intestines into the blood. Malabsorption may occur if the nutrients aren’t broken down into small enough bits and pieces, or it can happen if the walls of the small intestine become damaged. General symptoms of malabsorption can include diarrhea, bloating, fluid retention, and flatulence, and over time can lead to weakness, fatigue, muscle wasting, weight loss and various conditions specific to whatever vitamins or minerals aren’t absorbed.
The medical treatment for malabsorption syndrome depends on what’s causing the malabsorption; sometimes the main treatment is to make dietary changes, and no medication is necessary. For example, Celiac disease involves the inability to absorb fats and vitamins-soluble when the walls of the small intestine become damaged by an autoimmune reaction to gluten, a protein found in wheat, barley, and rye. Currently, the only treatment for celiac disease is to avoid eating foods with gluten, which allows the intestinal tissue to heal. You can’t really avoid diseases like celiac disease or pernicious anemia, but following your doctor’s advice is essential for getting all the nutrients you need. Sometimes you can prevent malabsorption problems. Avoid excessive use of laxatives or alcohol, both of which are associated with a higher risk of malabsorption syndromes. In other cases, medical treatment is necessary, and you’ll also need to take specific dietary supplements to replace nutrients you can’t absorb. The supplements need to be formulated so that they’re easy to digest and absorb. In some cases, the nutrients will need to be given intravenously, along with fluid if you’ve become dehydrated.
for more info
https://www.encyclopedia.com/medicine/diseases-and-conditions/pathology/malabsorption-syndrome
Tracheal stenosis is a narrowing of the trachea, or “windpipe”. Tracheal stenosis causes shortness of breath, which is made worse during Noisy breathing can be heard when tracheal stenosis is severe.  Or (narrowing due to a birth defect) is a rare condition in which the cartilage support structure of the trachea can cause a narrowing of the airway. A normal tracheal cartilage is C-shaped with a softer, posterior membrane which consists of muscle. Abnormalities of this cartilage can include tracheal cartilaginous sleeves, prone to obstruction and crusting, and complete tracheal rings, in which the trachea consists of several or more complete rings of cartilage with a narrowed diameter. Symptoms of tracheal stenosis can be present shortly after birth affected children may present with rapidly worsening symptoms in the face of an upper respiratory infection. Evaluation for tracheal stenosis may include X-rays and more advanced imaging such as CT or MR imaging. Imaging can provide information not only about the extent of airway narrowing.
Or (narrowing due to a birth defect) is a rare condition in which the cartilage support structure of the trachea can cause a narrowing of the airway. A normal tracheal cartilage is C-shaped with a softer, posterior membrane which consists of muscle. Abnormalities of this cartilage can include tracheal cartilaginous sleeves, prone to obstruction and crusting, and complete tracheal rings, in which the trachea consists of several or more complete rings of cartilage with a narrowed diameter. Symptoms of tracheal stenosis can be present shortly after birth affected children may present with rapidly worsening symptoms in the face of an upper respiratory infection. Evaluation for tracheal stenosis may include X-rays and more advanced imaging such as CT or MR imaging. Imaging can provide information not only about the extent of airway narrowing.
Endoscopic view of tracheal stenosis
For more help contact Tracheal Stenosis Foundation Click photo to enlarge it
https://www.facebook.com/stopts.org
Pyloric Stenosis
Pyloric stenosis, also called infantile hypertrophic pyloric stenosis, is a condition caused by an enlarged pylorus. The pylorus is a muscle that opens and closes to allow food to pass through the stomach into the intestine. When this muscle becomes enlarged, feedings are blocked from emptying out of the stomach. The retained feedings cause the infant to vomit.
What causes pyloric stenosis?
There is no known reason for enlargement of the pylorus. The main symptom of pyloric stenosis is vomiting undigested breast milk or formula soon after a feeding. Vomiting usually begins at four weeks of age but can happen as early as two weeks after birth. Once vomiting begins it becomes more frequent, and severe, and is often described as “forceful” or “projectile”. Infants with pyloric stenosis may become fussy and, since they cannot keep down all their feedings, are hungry between feedings and are not able to gain weight normally. If the vomiting continues infants may become ill from dehydration.
Pyloric stenosis is one of the most common conditions requiring surgery in infants. It is more common in boys than girls and usually affects children who are born at full term. It rarely occurs in premature infants. Although not thought to be hereditary, pyloric stenosis occurs more commonly in children of parents who had pyloric stenosis themselves as infants.
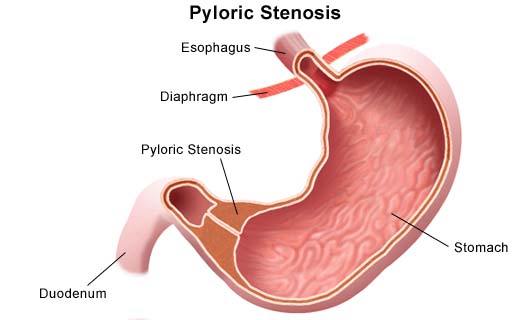 How is pyloric stenosis diagnosed?
How is pyloric stenosis diagnosed?
An examination of the abdomen may allow the doctor to feel the enlarged pyloric muscle (called an “olive”). If the pylorus cannot be felt, pyloric stenosis can be diagnosed by ultrasound study or by x-rays taken after the infant drinks a liquid called “contrast.” This is a study which examines the stomach and small intestine and is called an upper GI.
How is pyloric stenosis treated?
Pyloric stenosis does not get better by itself and must be corrected with an operation. The operation is called a “pyloromyotomy” where the surgeon cuts through the muscle fibres of enlarged pyloric muscle in order to widen the opening into the intestine. Prior to the operation, your child will be admitted to the hospital for intravenous fluids. Feedings will be held temporarily and restarted after the operation. A blood sample will be taken to check for dehydration and electrolyte abnormalities. Electrolytes measure the amount of sodium, potassium, carbon dioxide and chloride in the blood. The surgeon will schedule the operation as soon as the infant’s electrolyte levels are normal and the dehydration is corrected. This may take a day of treatment with intravenous fluids. A pyloromyotomy can be done using a small telescope and two miniature instruments through several small band-aid sized incisions, or it can be done through a very small incision on the abdomen.
http://pedsurg.ucsf.edu/conditions–procedures/pyloric-stenosis.aspx
Hypertrophic pyloric stenosis (HPS) is commonly encountered in pediatric practice. The typical infant presents with nonbilious projectile vomiting and dehydration (with hypochloremic hypokalemic metabolic alkalosis) if the diagnosis is delayed. Premature infants tend to present at 3-6 weeks from birth—not at 3-6 weeks from the due date—and these infants may have borderline normal muscle thickness because they are comparatively smaller. Hypertrophic pyloric stenosis is rarely seen in children older than 6 months.
This condition accounts for one-third of nonbilious vomiting occurrences in infants and is the most common reason for laparotomy before age 1 year. A striking male preponderance is seen, with a male-to-female ratio of 4-6:1. In addition, pyloric stenosis and,
(CLICK ON THIS READ WRITING) oesophagal atresia may coexist.
What Is Annular Pancreas?
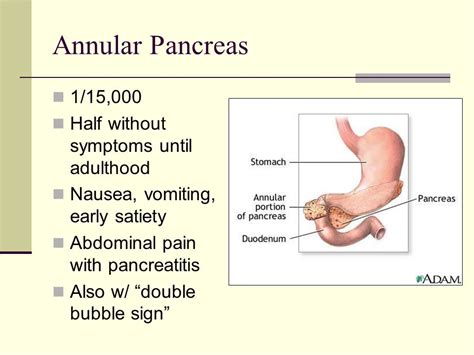 The pancreas is an organ in the posterior (back) of your abdomen, just behind the stomach. A duct connects the pancreas to a part of the small intestine called the duodenum. It is responsible for excreting insulin into the bloodstream to transform glucose into energy. It also secretes enzymes into the intestines to directly aid in the digestion of food.
The pancreas is an organ in the posterior (back) of your abdomen, just behind the stomach. A duct connects the pancreas to a part of the small intestine called the duodenum. It is responsible for excreting insulin into the bloodstream to transform glucose into energy. It also secretes enzymes into the intestines to directly aid in the digestion of food.
Normally, your pancreas sits next to your duodenum in your abdomen. In some people, tissue from the pancreas may surround the duodenum. When this happens, your duodenum can become restricted or blocked. This may impact your ability to digest food. This condition is known as annular pancreas.
What Are the Causes of Annular Pancreas?
Down’s syndrome.
tracheoesophageal fistula, an abnormal connection between the oesophagus and the trachea.
intestinal atresia, the failure of a portion of the intestinal tract to completely form.
pancreas divisum, a birth defect in which ducts of the pancreas don’t join together.
The annular pancreas also occurs with polyhydramnios, or excess amniotic fluid during pregnancy. Annular pancreas is a rare condition that occurs in only 1 in every 20,000 newborns. It occurs more frequently in males than in females.
For more on this click below
Note I couldn’t find a lot on this
 Introduction: GERD is a highly prevalent disease process and, with the advent of PPI, it has been successfully treated with medical management. In those patients that fail maximal medical management, Nissen fundoplication is the procedure of choice. Following a failed fundoplication, an acid-diverting procedure like RYGB is highly successful.
Introduction: GERD is a highly prevalent disease process and, with the advent of PPI, it has been successfully treated with medical management. In those patients that fail maximal medical management, Nissen fundoplication is the procedure of choice. Following a failed fundoplication, an acid-diverting procedure like RYGB is highly successful.
Materials and Methods: A 60-year-old male with a past medical history of fibromyalgia, arthritis, anxiety, depression, aspiration pneumonia, presented with a history of severe, longstanding GERD with aspiration and dysphagia; he had failed maximal medical therapy and a Nissen fundoplication.
The patient underwent a laparoscopic Roux –en –Y gastric bypass as an acid-diverting procedure. Intraoperative findings were large amounts of adhesions between the colon, small bowel, omentum, stomach, liver, and abdominal wall. An intraoperative EGD was performed in order to identify the GE junction. The hiatus was closed. An ante colic side-to-side gastrojejunostomy between the pouch and alimentary limbs was performed on the posterior wall with a linear stapler, on the anterior wall with a double layer of interrupted sutures, and checked for leakage with air. A side-to-side jejunojejunostomy between the biliopancreatic and alimentary limbs was performed 100 cm from the gastrojejunostomy. The patient tolerated the procedure well.
Result: The recovery of the patient was uneventful, with a normal UGI on POD2 without leak or obstruction. The patient noted that his symptoms of reflux and aspiration improved dramatically.
Conclusion: Roux-en-Y gastric bypass has been shown to be the most effective bariatric procedure that consistently leads to weight reduction and improvement of GERD symptoms. RYGB is the procedure of choice for patients with intractable GERD, following failed standard fundoplication procedures.
Billroth I or II anastomosis is mostly applied for distal gastrectomy. However reflux of duodenal contents into remnant stomach even oesophagus and extra-esophagus can be a challenging problem after the procedure.
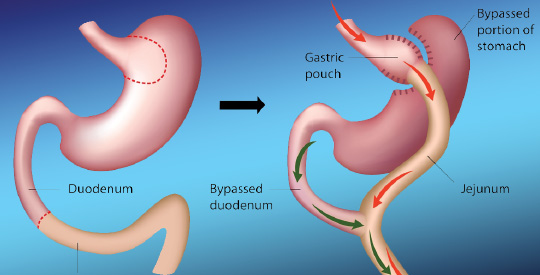 The erosive duodenal mixed with gastric fluid is much harmful to the end organ mucosa causing severe digestive even respiratory symptoms or complications. The main medication for gastroesophageal reflux disease (GERD), often a proton pump inhibitor (PPI), is often found to have limited effect for duodenal gastroesophageal reflux (DGER) .
The erosive duodenal mixed with gastric fluid is much harmful to the end organ mucosa causing severe digestive even respiratory symptoms or complications. The main medication for gastroesophageal reflux disease (GERD), often a proton pump inhibitor (PPI), is often found to have limited effect for duodenal gastroesophageal reflux (DGER) .
Laparoscopic fundoplication has been proved highly effective and becoming a standard antireflux procedure for GERD, however, a fundoplication may not sufficient to stop DGER, so we added Roux-en-Y diversion to the procedure. The purpose of this report is to describe the outcome of laparoscopic Dor fundoplication plus Roux-en-Y diversion in six patients with intractable duodenogastroesophageal reflux after Billroth I and II reconstruction.
For the full PDF click here and enlarge on their site
http://www.clinicsinsurgery.com/pdfs_folder/cis-v1-id1015.pdf
http://www.americanjournalofsurgery.com/article/S0002-9610(03)00213-7/abstract
Responsive website designed & developed by
![]()