Born unable to swallow, My Baby can not eat
Gastroschisis is a birth defect that develops in a baby while a woman is pregnant. This condition occurs when an opening forms in the baby’s abdominal wall. The baby’s bowel pushes through this hole. It then develops outside of the baby’s body in the amniotic fluid.
The opening is most often on the right side of the baby’s belly button. It can be large or small, but is typically 1-2 inches in size. In more severe cases, the stomach and/or liver can sometimes make their way through the opening as well.
Because the bowel is outside of the baby’s body, it is unprotected. That means there is a chance it can become irritated, swollen and damaged.
This condition is relatively rare, but has seen an increase in recent years. It occurs in about one in every 2,000 babies. It develops early in pregnancy, during the fourth through eighth weeks. Gastroschisis occurs due to a weakness in the baby’s abdominal wall muscles near the umbilical cord. If your baby develops this condition during your pregnancy, you will not experience any symptoms related to it.
Gastroschisis can be repaired with surgery after your baby is born. It is usually not associated with other malformations.
What Causes Gastroschisis?
The exact cause of gastroschisis is not known. It does not appear to be inherited. Having one baby with gastroschisis does not make it more likely that you would have another baby with the condition.
For more help understanding this
https://www.cincinnatichildrens.org/health/g/gastroschisis/
For a Facebook Group
https://www.facebook.com/averysangels
Support website// http://averysangels.org/
What is Vesicoureteral Reflux?
Normally, urine flows one way, down from the kidneys, through tubes called ureters, to the bladder. But what happens when urine flows from the bladder back into the ureters? This is called vesicoureteral reflux. With vesicoureteral reflux, urine flows backward from the bladder, up the ureter to the kidney. It may happen in one or both ureters. When the “flap valve” doesn’t work and lets urine flow backward, bacteria from the bladder can enter the kidney. This may cause a kidney infection that can cause kidney damage. When the flow of urine back up the ureters is more severe, the ureters and kidneys become large and twisted. More severe reflux is tied to a greater risk of kidney damage if there is an infection present.
With photo’s
http://www.urologyhealth.org/urologic-conditions/vesicoureteral-reflux-(vur)
http://emedicine.medscape.com/article/1016439-overview
What are the types of VUR?
The two types of VUR are primary and secondary. Most cases of VUR are primary and typically affect only one ureter and kidney. With primary VUR, a child is born with a ureter that did not grow long enough during the child’s development in the womb. The valve formed by the ureter pressing against the bladder wall does not close properly, so urine refluxes from the bladder to the ureter and eventually to the kidney. This type of VUR can get better or disappear as a child gets older. As a child grows, the ureter gets longer and function of the valve improves.
Secondary VUR occurs when a blockage in the urinary tract causes an increase in pressure and pushes urine back up into the ureters. Children with secondary VUR often have bilateral reflux. VUR caused by a physical defect typically results from an abnormal fold of tissue in the urethra that keeps urine from flowing freely out of the bladder.
VUR is usually classified as grade I through V, with grade I being the least severe and grade V being the most severe.
With Photo’s
Born unable to swallow, My Baby can not eat
Acid Reflux and Shortness of Breath June 15, 2015
Part 1 of 4: Overview
Difficulty breathing is one of the more frightening symptoms of acid reflux and the chronic form of the condition, which is called gastroesophageal reflux disease (GERD). GERD can be associated with breathing difficulties such as bronchospasm and aspiration. These difficulties can sometimes lead to life-threatening respiratory complications.
Shortness of breath, also called dyspnea, occurs with GERD because stomach acid that creeps into the esophagus can cause it to narrow. When gastric acid reaches the vocal folds, airways, and lungs, it can cause a swelling of the passages. This can lead to atypical asthma reactions. Such airway damage can affect breathing by causing coughing or wheezing and making swallowing solid foods more difficult.
http://www.healthline.com/health/gerd/shortness-of-breath#Overview1
Post Nasal Drip
A relatively common disorder among people with allergies and other conditions like acid reflux
A relatively common disorder among people with allergies and other conditions like acid reflux is a post-nasal drip. A post-nasal drip has several causes and symptoms that can disrupt your day and cause discomfort. Like any medical condition, it is important to get this treated right away if you have it. Knowing post-nasal drip symptoms helps toward identifying what is wrong and being able to tell a doctor what you are experiencing. Post-nasal drip symptoms are varied and can last a long time if they are not identified and treated. Some of the most severe signs of post-nasal drip (click on red writing) are similar to the signs of normal allergy irritation and may be ignored by some people. If you know the symptoms for this condition and experience any of them, it is important to let your doctor know.
One of the most common and severe post-nasal drip symptoms is coughing. People with a post-nasal drip tend to start out with a mild cough that is commonly mistaken for a cough from allergies or irritation. This cough can become severe and in some cases painful. Coughing associated with post nasal drip tends to be persistent and is often accompanied by wheezing. Wheezing is more commonly from the presence of post nasal drip than asthma. The excess mucus from post-nasal drip can cause you to wheeze and cough frequently and the symptoms will not subside until the drip is corrected.
http://www.therabreath.com/how-to-stop-post-nasal-drip.html
Airway reflux as a cause of respiratory disease.
Summary Reflux is the cause of much respiratory disease. More commonly still, it is the unrecognized agent provoking the symptoms of respiratory disease. That the reflux entering the airways from the gastrointestinal tract is central to the diagnosis, therapy, and understanding of respiratory pathology has been missed because the paradigm of a peptic disease has been applied. Airway reflux is however unlike gastro-oesophageal reflux disease (GORD). GORD is liquid acid reflux causing heartburn and indigestion. Airway reflux consists of a mainly gaseous non-acid mist which, when deposited in the upper and lower airways leads to inflammation, fibrosis, bronchoconstriction, and cough. Here, the hypothesis that airway reflux is responsible for chronic “idiopathic” a cough, late-onset asthma, exacerbations of COPD, ‘idiopathic’ pulmonary fibrosis and even the lung disease of cystic fibrosis is outlined. The exclusive focus of clinicians on the extrinsic origins of these conditions and the rejection of an obvious intrinsic etiology causes millions of patients to be denied an explanation for their symptoms and simple, effective, treatments. In many cases, idiopathic should be no longer considered idiopathic.
Introduction
Reflux is the cause of all respiratory disease. An exaggeration of course, but I hope to convince you in this article that there is more than a germ of truth in this outrageous statement. There have been two barriers to the revelation that reflux is a major contributor to respiratory pathology. First, we have been laboring under the diagnostic criteria of reflux as gastroesophageal reflux disease (GORD). There is no doubt that GORD exists and the gastroenterologists have defined and characterized the disease which causes heartburn, dyspepsia, and oesophagitis; however, they have been very reluctant to accept that this is merely the tip of the reflux iceberg, with extra-oesophageal reflux being out of their home territory. Respiratory professionals, being largely ignorant of reflux, its etiology and manifestations, have accepted the wisdom of the gastroenterologists since this is “their” area. So blinkered has this attitude become that, with one or two exceptions, one should not talk to a gastroenterologist about what has been termed airway reflux. You might as well talk to a tree!
http://breathe.ersjournals.com/content/9/4/256
A hiatus hernia is when part of the upper stomach slides upwards into the chest. It does this by pushing through the natural opening in the diaphragm muscle through which the esophagus (the pipe that goes from the mouth to the stomach) passes. Hiatus hernias are common, especially in people over 50.
Your stomach usually sits completely below your diaphragm. The diaphragm is the sheet of muscle that separates your chest (where your lungs and heart are) from your abdomen (tummy).
our diaphragm has an opening in it called the hiatus. Your esophagus passes through the hiatus. A hiatus hernia develops when part of your stomach slides back up through the hiatus and into your chest.
A hiatus hernia is very common – around three in 10 people over 50 will get it. However, this number may be higher, because many people with a hiatus hernia have very mild symptoms or none at all, and may not realize that they have the condition.
How a sliding hiatus hernia forms
When the junction between the esophagus and the stomach, as well as a portion of the stomach itself, slides up above the diaphragm.
There are two types of a hiatus hernia, a sliding hiatus hernia and a rolling hiatus hernia. Around nine out of 10 people with a hiatus hernia have the sliding type. This is when both the stomach and the junction where your oesophagus and stomach meet slide upwards into your chest. A rolling hiatus hernia is where just part of your stomach pushes up into the chest.
How a rolling hiatus hernia forms
When a portion of your stomach goes through the diaphragm and lies beside the oesophagus.
Most hiatus hernias don’t cause any symptoms. If you do get symptoms, they are unlikely to be serious.
A sliding hiatus hernia can cause a problem called gastro-oesophageal reflux disease (GORD). This is when acid or bile in the stomach rises back up into your oesophagus.
The most common symptom of GORD is heartburn, which causes a warm or burning sensation in your chest. The burning feeling from heartburn can go all the way up to your throat. You may be more likely to notice heartburn after smoking, drinking alcohol or coffee, or eating chocolate. It can also get worse when you bend over or when you’re lying down.
Other symptoms of a hiatus hernia and GORD include:
- feeling sick or being sick
- a cough or wheezing when breathing, especially at night – this is caused by breathing in the acid that has come up from your stomach
- your mouth filling with saliva
- finding it difficult or painful to swallow
You can have a hiatus hernia without GORD, and you can have GORD without having a hiatus hernia, but they often go together.
Treatment for a hiatus hernia generally aims to ease the symptoms of acid reflux. The treatment you need will depend on how severe your symptoms are and how much they are affecting you.
Self-help
You can reduce the symptoms of a hiatus hernia and prevent further problems by making the following lifestyle changes.
- If you’re overweight or obese, lose excess weight.
- Eat small meals often and try not to eat just before you go to bed.
- Giving up smoking and cutting down on alcohol will help.
- Wear loose comfortable clothes.
- Raise the head of your bed and try not to stoop or bend down.
- Cut down or stop eating food or drinks that make your symptoms worse. See our frequently asked questions for more information.
Medicines
You can take medicines to help reduce the symptoms of reflux from a sliding hiatus hernia. The most common are antacids, which work by neutralizing the acid in your stomach. How well antacids work varies from person to person. If you find they don’t relieve your symptoms, your GP or pharmacist may suggest a different medicine. The two main types that you may be prescribed are called H2 receptor antagonists and proton pump inhibitors. Both of these reduce the amount of acid produced by your stomach.
Surgery
If you have tried other treatments and they haven’t worked, or your symptoms are severe, your doctor may suggest an operation. You will also need to have surgery if a rolling hernia becomes strangulated.
There are a number of different types of operation to repair a hiatus hernia. They involve putting the gastro-oesophageal junction back into your abdomen and tightening up the hiatus (the opening).
Your surgeon will also strengthen the esophageal sphincter by wrapping the stomach around it. The oesophageal sphincter is a bundle of muscles which stops what is in your stomach from coming back out. This operation is called a fundoplication and is usually done as a laparoscopic (keyhole) procedure.
Dysmotility is a condition in which muscles of the digestive system become impaired and changes in the speed, strength or coordination in the digestive organs occurs. In the normal.
small intestine, liquefied food and secretions including digestive enzymes are pushed onwards by waves of muscular contraction. When these contractions are impaired, the contents are trapped and cause distention with symptoms such as bloating, nausea, vomiting and even malnutrition. There are many causes of abnormal intestinal motility that can be separated into two different groups.
www.ddc.musc.edu/public/organs/smallBowel.html
abnormalities of the muscle of the intestine (myopathy)
abnormalities in the neural (nerve) control of the muscle (neuropathy)
Nerve and muscle abnormalities may be genetically inherited. In this situation, it is common to find many patients’ family members with contraction problems, not only of the intestinal muscle but also of the bladder. There are secondary causes of intestinal dysmotility. Examples of this include systemic Lupus erythematosus, amyloidosis, neurofibromatosis, Parkinson’s disease, diabetes, scleroderma, thyroid disorders, and muscular dystrophies. Certain medications can also cause intestinal dysmotility. Additionally, any disorders that cause inflammation to the intestine can cause significant dysmotility (i.e. radiation therapy, celiac disease)
www.ddc.musc.edu/public/symptomsDiseases/diseases/smallBowel/celiacSprue.html
www.ddc.musc.edu/public/symptomsDiseases/diseases/smallBowel/amyloidosis.html
Symptoms may be absent or trivial. Some patients may have severe ongoing attacks due to a blockage is known as an intestinal pseudo-obstruction. Patients who develop bacterial overgrowth because of poor motility may develop diarrhoea, while others may be constipated. Associated disorders of motility in other organs such as the oesophagus, stomach and colon will produce other symptoms. Patients with severe dysmotility will develop malnutrition because they are unable to eat adequately.
Diagnosis
Blood Tests – Blood tests help to assess the degree of malnutrition, anaemia and any salt imbalance. They may also make a specific diagnosis such as diabetes, thyroid problems and systemic disorders such as Lupus.
X-ray Studies – X-ray studies (barium) help to delineate the extent of bowel involvement by demonstrating areas of distended intestines, and by excluding mechanical obstruction. This must be done because treatment of pseudo-obstruction and true obstruction are very different.
www.ddc.musc.edu/public/tests/diagnosticRadiology/bariumMeal.html
Motility/Transit Studies – Motility/transit investigations help to define the degree of contractile abnormality as well as a propulsive abnormality of the intestines. They are sometimes useful (by assessing the pattern of contraction) in deciding whether a neuropathy or myopathy is present.
Transit Time Measurement
A transit time X-ray measures the time it takes for food to go through the colon. The person takes special capsules by mouth twice a day for five days. Each capsule has twelve X-ray markers. Each day, the person takes a total of twenty-four markers. This averages out to one every hour.
The average normal transit time is thirty-five hours. The upper limit of normal is seventy-two hours. If it takes more than seventy-two hours to go through the body, and all other tests are normal, then we make the diagnosis of colonic inertia (slow transit).
www.ddc.musc.edu/public/symptomsDiseases/diseases/colon/colonicInertia.html
It is important to avoid the use of all laxatives and enemas during the five days before a transit time X-ray. However, it is fine to continue Natural Vegetable Powder, or other fiber supplements, in a normal dose.
Biopsies – Biopsy samples of the intestine are obtained at endoscopy or surgery, and may detect the cause of the dysmotility.
Treatment
Mechanical obstruction (i.e. blockage) must be excluded before a patient is diagnosed as having pseudo-obstruction or intestinal dysmotility as a cause of their symptoms. Specific treatments are available for some causes of dysmotility, including abnormalities in salt balance and endocrine problems such as thyroid disease.
Unfortunately, many causes of dysmotility cannot be cured, and symptomatic treatment is offered. Medicines can stimulate intestinal motility and help with propulsion of intestinal contents. Dietary modifications are advised. It is important that adequate calories are taken, usually in the form of meal supplements. Patients should avoid gas-forming foods, carbonated beverages, and foods that are difficult to digest. Patients may need to be admitted to hospital for intravenous fluids, and decompression of the intestine with a tube placed in the stomach. Occasionally, nutrition will have to be supplied through a vein.
When only a short segment of the small intestine is involved, surgical resection may be appropriate. However, patients must be carefully selected as surgery can lead to scarring (adhesions) within the abdominal cavity, with further disturbance of intestinal motility.
Schatzki rings are fixed anatomic mucosal ring structures in the distal esophagus. They are distinct from lower esophageal  muscular rings (A rings), which are transient, smooth, circumferential indentations in the esophagus. Lower esophageal rings were described first by Templeton in 1944. The vast majority of patients with lower esophageal rings are asymptomatic. In fact, lower esophageal rings are found during 6-14% of all routine upper gastrointestinal barium examinations. Lower esophageal rings that cause symptoms (true Schatzki rings) occur in only 0.5% of patients undergoing these examinations.
muscular rings (A rings), which are transient, smooth, circumferential indentations in the esophagus. Lower esophageal rings were described first by Templeton in 1944. The vast majority of patients with lower esophageal rings are asymptomatic. In fact, lower esophageal rings are found during 6-14% of all routine upper gastrointestinal barium examinations. Lower esophageal rings that cause symptoms (true Schatzki rings) occur in only 0.5% of patients undergoing these examinations.
Schatzki rings are a common cause of intermittent dysphagia. Barium esophagography is the preferred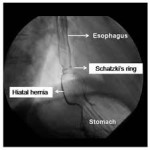 method of detection of Schatzki rings. Esophageal rings may be missed during barium esophagography if distention of the distal esophagus is inadequate; therefore, adequate distention of the esophagus during barium esophagography is imperative. A modified Valsalva maneuver also may help in demonstrating the ring by distending the associated hiatal hernia. (As seen above on this page) Some people may have a Schatzki’s ring since birth. Sometimes, it is due to Gastro Esophageal Reflux Disease (GERD).
method of detection of Schatzki rings. Esophageal rings may be missed during barium esophagography if distention of the distal esophagus is inadequate; therefore, adequate distention of the esophagus during barium esophagography is imperative. A modified Valsalva maneuver also may help in demonstrating the ring by distending the associated hiatal hernia. (As seen above on this page) Some people may have a Schatzki’s ring since birth. Sometimes, it is due to Gastro Esophageal Reflux Disease (GERD).
Structuring, or narrowing, can be caused by acid in the stomach entering up into the esophagus causing the esophagus tissue to scar. Scar tissue may develop into a narrowing or tightness that could form a structure which sometimes causes food, pills and/or liquids to get stuck.
For more on this
http://www.gandhofcny.com/education/diseases/esophageal-ring-stricture/
http://healthool.com/schatzki-ring/
Read from Patient’s themselves
http://www.medicinenet.com/schatzki_ring/patient-comments-1645.htm
The most famous and common ring in the esophageal is the B ring or Schatzki ring. The pathogenesis and treatment of oesophagal rings and webs are evolving. Most of these structural lesions are asymptomatic but can cause dysphagia. Some 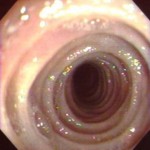 authors believe the Schatzki ring is a protective barrier against gastroesophageal reflux (GER) Esophageal rings usually exist as a single lesion but can be multiple, as shown in the photo on left. Several names have been coined for when multiple rings are found in the esophageal, including multiple esophageal rings or webs, congenital esophageal stenosis, ringed esophageal, corrugated esophageal, and feline esophageal. Esophageal rings and webs are folds that block your esophageal either partially or completely. Rings are bands of normal esophageal tissue that form constrictions around the inside of the esophageal. They occur in the lower esophagus. Webs, which arise in the upper esophagus, are thin layers of cells that grow across the inside of the esophagus. Either condition may make it difficult to swallow solid food. Experts aren’t sure what causes esophageal rings and webs. The condition may be congenital (inherited) or may develop after birth. Most esophageal rings and webs do not cause any symptoms and are discovered when people have barium X-rays or endoscopy for unrelated reasons. When rings or webs do cause symptoms, the most common complaint is difficulty swallowing solids. Foods, especially meats and pieces of bread, may feel like they get stuck in the same place. People with esophageal rings and webs commonly have reflux symptoms. When esophageal webs occur together with iron deficiency anemia the condition is known as Plummer-Vinson syndrome.
authors believe the Schatzki ring is a protective barrier against gastroesophageal reflux (GER) Esophageal rings usually exist as a single lesion but can be multiple, as shown in the photo on left. Several names have been coined for when multiple rings are found in the esophageal, including multiple esophageal rings or webs, congenital esophageal stenosis, ringed esophageal, corrugated esophageal, and feline esophageal. Esophageal rings and webs are folds that block your esophageal either partially or completely. Rings are bands of normal esophageal tissue that form constrictions around the inside of the esophageal. They occur in the lower esophagus. Webs, which arise in the upper esophagus, are thin layers of cells that grow across the inside of the esophagus. Either condition may make it difficult to swallow solid food. Experts aren’t sure what causes esophageal rings and webs. The condition may be congenital (inherited) or may develop after birth. Most esophageal rings and webs do not cause any symptoms and are discovered when people have barium X-rays or endoscopy for unrelated reasons. When rings or webs do cause symptoms, the most common complaint is difficulty swallowing solids. Foods, especially meats and pieces of bread, may feel like they get stuck in the same place. People with esophageal rings and webs commonly have reflux symptoms. When esophageal webs occur together with iron deficiency anemia the condition is known as Plummer-Vinson syndrome.
The association of postcricoid dysphagia, upper esophageal webs, and iron deficiency anemia are known as Plummer-Vinson syndrome (PVS) in the United States and Paterson-Brown-Kelly syndrome in the United Kingdom. The term sideropenic dysphagia has also been used because the syndrome can occur with iron deficiency (sideropenia), but it is not associated with anemia.
Cricoid ring 2017
Background:
Knowledge regarding the shape, size, and variability of the cricoid ring is important to properly choose the correct endotracheal tube (ETT) in the pediatric patient. Studies have measured the size of the cricoid ring using methodologies such as moulages, magnetic resonance imaging, and video-bronchoscopy. In the present study, computed tomography (CT) -based images were used to determine the shape, size, and configuration of the cricoid ring in the pediatric population taking into considerations growth and development. This is a retrospective review using 130 CT images of children ranging in age from 1 month to 10 years undergoing radiological evaluation unrelated to airway symptomatology. The CT scans were obtained in spontaneously breathing patients during either natural sleep or procedural sedation. Anteroposterior (AP) and transverse (T) diameters were measured at the cricoid ring using these images.
READ FULL Report here very long


