Hannah Warren has been unable to breathe, eat, drink or swallow on her own since she was born in South Korea in 2010. Until the operation at a United States hospital, she had spent her entire life in a hospital in Seoul. Doctors there told her parents there was no hope and they expected her to die.
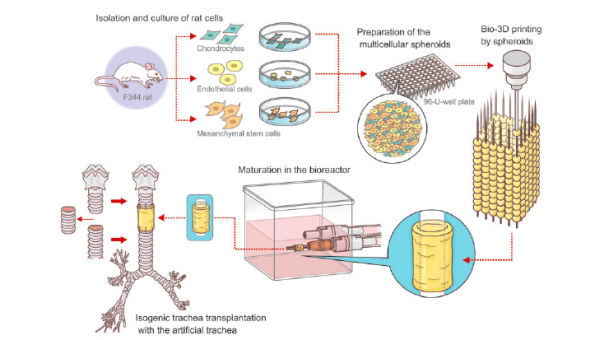
The stem cells came from Hannah’s bone marrow, extracted with a special needle inserted into her hip bone. They were seeded in a lab onto a plastic scaffold, where it took less than a week for them to multiply and create a new windpipe.
About the size of an 8cm tube of penne pasta, it was implanted on April 9 in a nine-hour procedure.
Early signs indicate the windpipe is working, Hannah’s doctors announced Tuesday, although she is still on a ventilator. They believe she will eventually be able to live at home and lead a normal life.
 “We feel like she’s reborn,” said Hannah’s father, Darryl Warren.
“We feel like she’s reborn,” said Hannah’s father, Darryl Warren.
“They hope that she can do everything that a normal child can do but it’s going to take time. This is a brand new road that all of us are on,” he said in a telephone interview. “This is her only chance but she’s got a fantastic one and an unbelievable one.”
Only about one in 50,000 children worldwide are born with the same defect. The stem-cell technique has been used to make other body parts besides windpipes and holds promise for treating other birth defects and childhood diseases, her doctors said.
The operation brought together an Italian surgeon based in Sweden who pioneered the technique, a pediatric surgeon at Children’s Hospital of Illinois in Peoria who met Hannah’s family while on a business trip to South Korea, and Hannah – born to a Newfoundland man and Korean woman who married after he moved to that country to teach English.
Hannah’s parents had read about Dr. Paolo Macchiarini’s success using stem-cell based tracheas but couldn’t afford to pay for the operation at his center, the Karolinska Institute in Stockholm. So Dr. Mark Holterman helped the family arrange to have the procedure at his Peoria hospital, bringing in Macchiarini to lead the operation. Children’s Hospital waived the cost, likely hundreds of thousands of dollars, Holterman said.